Discover and read the best of Twitter Threads about #FOAMcc
Most recents (24)
Toxicologists are often consulted about 🍄foraging misadventures (wild mushroom ingestion).
Usually you don't get a clear mushroom image like this video (at best a blurry photo of some OTHER mushroom), or more often no image.
So what to do?
A 🍄🧵
#FOAMed #FoamCC #MedEd
Usually you don't get a clear mushroom image like this video (at best a blurry photo of some OTHER mushroom), or more often no image.
So what to do?
A 🍄🧵
#FOAMed #FoamCC #MedEd
If you do have a good sample or photo you can work with a mycologist (your posion center knows one) to identify the shroom. But this is not frequent.
Since we almost never have that we usually rely on history and symptoms
Key to differentiating mushroom toxicity types: time to onset of GI issues. Most mushrooms upset the tummy. The 5hr “rule” helps identify bad ones.
Key to differentiating mushroom toxicity types: time to onset of GI issues. Most mushrooms upset the tummy. The 5hr “rule” helps identify bad ones.
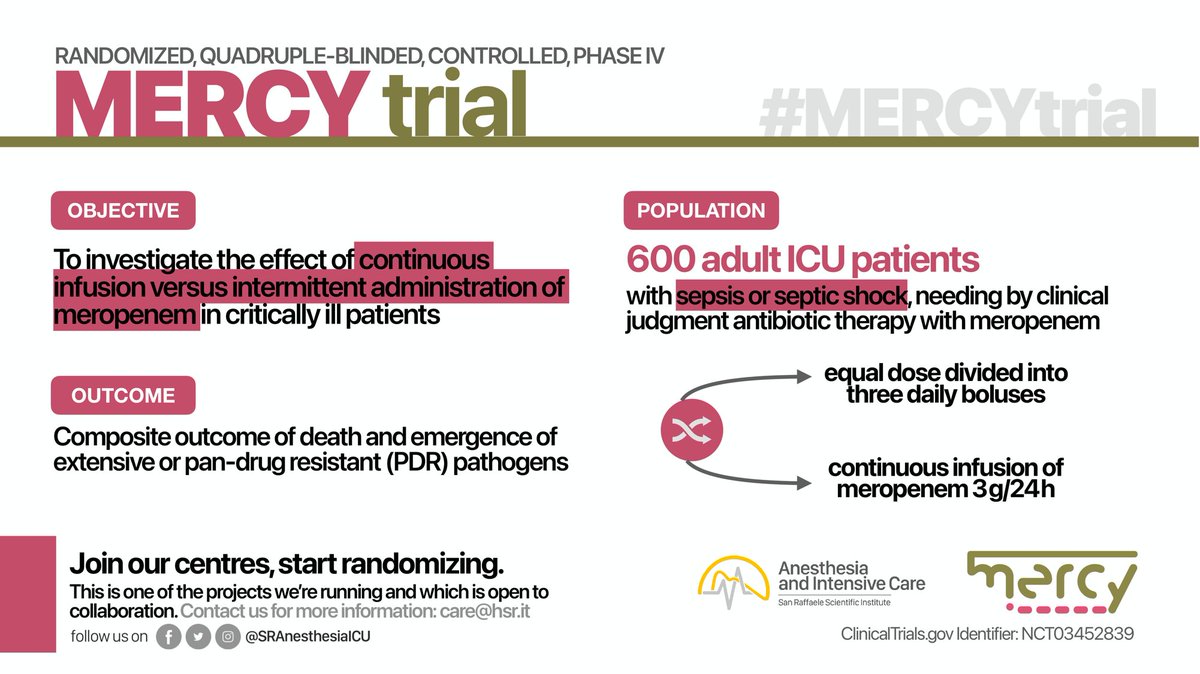
We've just presented and published a multicenter RCT at #CCR23 and in @JAMA_current!
Continuous vs Intermittent Meropenem Administration in Critically Ill Patients with Sepsis: The #MERCYtrial!
🔗 jamanetwork.com/journals/jama/…
This 🧵 will explain the study in detail /11
#FOAMcc
Continuous vs Intermittent Meropenem Administration in Critically Ill Patients with Sepsis: The #MERCYtrial!
🔗 jamanetwork.com/journals/jama/…
This 🧵 will explain the study in detail /11
#FOAMcc
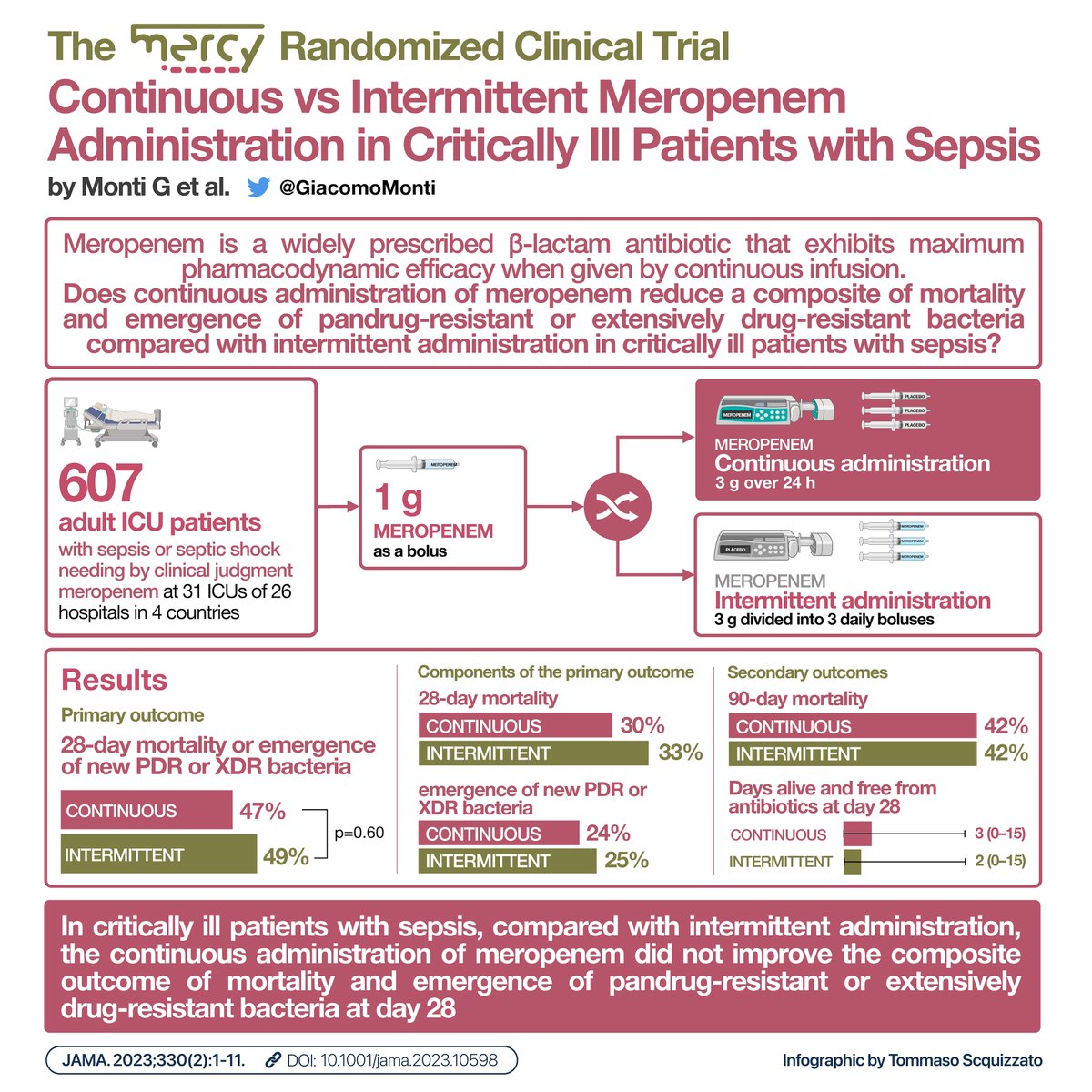
2/
β-lactams (e.g., #meropenem), are typically given intermittently, but continuous administration can provide constant serum levels and may improve outcomes.
In fact, several meta-analyses reported reduced mortality when administered continuously.
β-lactams (e.g., #meropenem), are typically given intermittently, but continuous administration can provide constant serum levels and may improve outcomes.
In fact, several meta-analyses reported reduced mortality when administered continuously.

3/
Therefore, we conducted a multinational, double-blind, randomized controlled trial to test the hypothesis that continuous administration of #meropenem, compared with intermittent administration, would improve clinically relevant outcomes in critically ill pts with #sepsis
Therefore, we conducted a multinational, double-blind, randomized controlled trial to test the hypothesis that continuous administration of #meropenem, compared with intermittent administration, would improve clinically relevant outcomes in critically ill pts with #sepsis
ICU stories (common): Middle-aged pt w hx of COPD was brought to the ED by EMS after SOB x 2 days. No fever or chest pain. Very quickly after ED arrival, he was intubated. CXR showed hyperinflated, “COPD” lungs. Here depicted in two images: 



BP dropped post-intubation to 55/40; propofol was started & then discontinued due to hypotension. iv fluids (2L Lactate Ringer's) were started & patient was brought to the ICU w SBP in upper 80s. Re-institution of propofol led again to hypotension. What would be the next step?
ICU pictorials: A patient was admitted for "weakness". Unimpressive vitals / phys exam / labs. A few days later because of temp 101 F, a fever w/u was initiated. Due to "SOB", a CT chest angio was done:
Echo findings:
ICU Quizzes:
What is the most common electrolyte abnormality seen in the hospital?
What is the most common electrolyte abnormality seen in the hospital?
👆 C.
In what time frame of development, is a hyponatremic episode considered acute?
In what time frame of development, is a hyponatremic episode considered acute?
👆 C.
If the onset of hyponatremia is unknown, it should be managed as:
If the onset of hyponatremia is unknown, it should be managed as:
I was checking again today about DKA/HHS in a very modern & easy to read textbook and I saw this about the Na correction: 

The Katz correction factor is 1.6 mEq/L for every 100 mg/dL that the serum Glu exceeds 100 mg/dL & the Hillier correction factor is 2.4 mEq/L
amjmed.com/article/S0002-…
amjmed.com/article/S0002-…
It seems that the textbook 👆 uses a sodium correction factor of < 1.0 mEq/L for every 100 mg/dL of Glu above 100 or applies the correction starting from a higher Glu level (probably 200 mg/dL?)
1/
Second day of @Smart_Meeting_M
Professor @giovannilandoni talking about management of #anticoagulant in #perioperative patients 💉
✅You surely all know how to deal with #antithrombotic and #regionalanesthesia, here the guidelines:
pubmed.ncbi.nlm.nih.gov/34980845/
#FOAMed #FOAMcc
Second day of @Smart_Meeting_M
Professor @giovannilandoni talking about management of #anticoagulant in #perioperative patients 💉
✅You surely all know how to deal with #antithrombotic and #regionalanesthesia, here the guidelines:
pubmed.ncbi.nlm.nih.gov/34980845/
#FOAMed #FOAMcc
2/
💡Let's focus on perioperative #DOAC /#NOAC / #TSOAC
➡️Consider both #surgical blood loss risk and #patient characteristics.
⚠️Remember NOT to bridge with #LMWH or #UFH.
pubmed.ncbi.nlm.nih.gov/33895845/
💡Let's focus on perioperative #DOAC /#NOAC / #TSOAC
➡️Consider both #surgical blood loss risk and #patient characteristics.
⚠️Remember NOT to bridge with #LMWH or #UFH.
pubmed.ncbi.nlm.nih.gov/33895845/

3/
What if it's not an elective patient??
Use #reversal agents when needed❗
🔹#Idarucizumab for #dabigatran
🔹#Andexanet for #apixaban and #rivaroxaban
💡#Prothrombin complex concentrates in addiction
pubmed.ncbi.nlm.nih.gov/36988142/
What if it's not an elective patient??
Use #reversal agents when needed❗
🔹#Idarucizumab for #dabigatran
🔹#Andexanet for #apixaban and #rivaroxaban
💡#Prothrombin complex concentrates in addiction
pubmed.ncbi.nlm.nih.gov/36988142/

ICU stories (last night): A patient had been admitted w pneumonia / intubated / on norepi 0.12. At 01:00 am, the nurse notifies you that urine output is 5-10 cc/hr for the previous 3 hours. BP is 99/44, HR 90, CRT 3 sec. You take the US in patient's room to see what's happening.
What POCUS finding(s) is/are likely to explain the oligo-anuria in the shortest amount of time?
If you (and the patient) are lucky, you may find this:
1/
🎬 Now on stage Professor @giovannilandoni talking about what we DON'T KNOW about #cardiocirculatory drugs
✅ #Norepineprhine is the most used vasoactive drug in the guidelines for:
🔹 #sepsis
🔹#cardiogenic shock❗(Scandinavian)
BUT...
@Smart_Meeting_M @SRAnesthesiaICU
🎬 Now on stage Professor @giovannilandoni talking about what we DON'T KNOW about #cardiocirculatory drugs
✅ #Norepineprhine is the most used vasoactive drug in the guidelines for:
🔹 #sepsis
🔹#cardiogenic shock❗(Scandinavian)
BUT...
@Smart_Meeting_M @SRAnesthesiaICU

2/
BUT... #Norepineprhine (base) does not exist❗
🚫 base is not soluble, unstable and unable to reach target receptors
💡 Let's make it a salt!
🤔 But which one?
⚠️ Available Norepineprhine salts has different #dilution
⚠️ Sometimes with misleading #labeling
BUT... #Norepineprhine (base) does not exist❗
🚫 base is not soluble, unstable and unable to reach target receptors
💡 Let's make it a salt!
🤔 But which one?
⚠️ Available Norepineprhine salts has different #dilution
⚠️ Sometimes with misleading #labeling

3/
➡️ Please do not change you're clinical practice for this ⬅️
But consider the possible implications on:
🔹Second line drugs initiation
🔹Co- administration of other vasopressors
❗Comunication of your results!!!
pubmed.ncbi.nlm.nih.gov/36978126/
#FOAMed #FOAMcc
➡️ Please do not change you're clinical practice for this ⬅️
But consider the possible implications on:
🔹Second line drugs initiation
🔹Co- administration of other vasopressors
❗Comunication of your results!!!
pubmed.ncbi.nlm.nih.gov/36978126/
#FOAMed #FOAMcc

ICU stories: Pt w "severe COPD" (ex-smoker; FEV1 30%) / chronic hypoxic-hypercapnic resp failure on 2-4 l/m O2 @ home / diastolic HF / HTN / HLD was brought to the ED due to "altered mental status" & "shortness of breath". S/he left the hospital 3-4 months ago after an episode
of "COPD exacerbation" (the 4th during the last 12 months). In the ED: sat in low 80s & after a brief non-rebreather mask trial, pt was placed on NIV. ABGs: PCO2>100 (above detection limit), pH 7.14, HCO3 undetectable. Pt suffered 2 grand mal seizures, & after receiving
lorazepam & 2l NS, s/he was intubated (roc+keta) & rushed to the ICU. Per ED: ECG w sinus tach & CXR "COPD lungs" & R basilar infiltrate. Labs: WBC 14K, creat 2.0 (baseline 1.4). You examine the pt quickly: sedated-?paralyzed/decr BS & wheezing bil/trace ext edema/skin not cold
#POCUS enthusiasts, is this IVC normal, abnormal? (asking about possibilities, not definitive conclusions)
#FOAMcc #MedEd #Nephpearls
(Transverse view in thread)
#FOAMcc #MedEd #Nephpearls
(Transverse view in thread)
IVC transverse #POCUS
#POCUS answer:
I deliberately avoided clinical context in the original tweet to gather multiple opinions.
Image obtained from a thin, trained athlete with resting HR in 40s-50s.
A dilated IVC is commonly seen in this setting with no right heart pathology. In addition, particulate… twitter.com/i/web/status/1…
I deliberately avoided clinical context in the original tweet to gather multiple opinions.
Image obtained from a thin, trained athlete with resting HR in 40s-50s.
A dilated IVC is commonly seen in this setting with no right heart pathology. In addition, particulate… twitter.com/i/web/status/1…

Deresuscitation has become more and more ubiquitous within ICU practice. But what tools can we use to do it? Over the next 2 Tweetorials, i’ll explain some pharmacological methods. Focussing on the JICS mix!
My talk from #ACCS2023
#FOAMed #POCUS #FOAMcc #medtwitter
My talk from #ACCS2023
#FOAMed #POCUS #FOAMcc #medtwitter
The brilliant paper in question is well worth a good read through. For both its novel description of combination diuretic therapy, and its golden descriptions of simple and complex fluid/renal physiology.
Here’s the infamous JICS mix:
journals.sagepub.com/doi/epdf/10.11…
Here’s the infamous JICS mix:
journals.sagepub.com/doi/epdf/10.11…

We know, universally, oedema on the ICU is contentious. Early goal directed therapy trials after Shoemaker, all demonstrated worse outcomes. Why?🤔
There were signals towards positive fluid balance and probably states of venous congestion in the treatment arms.
There were signals towards positive fluid balance and probably states of venous congestion in the treatment arms.
Why do we put tracheostomies in patients though?
The rationale for a trachy in ICU is that there are respiratory mechanical benefit (compare to a tracheal tube and a native airway). There are many patient care benefits - oral care, feeding, etc...
#VTA23
The rationale for a trachy in ICU is that there are respiratory mechanical benefit (compare to a tracheal tube and a native airway). There are many patient care benefits - oral care, feeding, etc...
#VTA23
There are problems, including the potential for real patient harm. Tracheostomy emergencies are a problem. Complications (Immediate, Early and Late) are encountered in 30% of patients. #VTA23
PEEP is important - it improves oxygenation, and is an essential component of lung protective strategies.
But PEEP also has some problems - it can cause hypotension and increased pulmonary vascular resistance.
So how does one get optimal PEEP?
#VTA23
But PEEP also has some problems - it can cause hypotension and increased pulmonary vascular resistance.
So how does one get optimal PEEP?
#VTA23
Optimal PEEP has no clear universal definition.
Maybe we should look for appropriate PEEP - a PEEP value that results in adequate oxygenation with the lowest risk of overdistension.
#VTA23
Maybe we should look for appropriate PEEP - a PEEP value that results in adequate oxygenation with the lowest risk of overdistension.
#VTA23
Prof Anthony Holley is speaking next on 'Respiratory Support in the Trauma Patient' #VTA23 #critcare #FOAMcc
The 'trauma' patient is not a single disease entity, but ultimately a mechanism that is characterised by a shared multitude of pathophysiological patterns (TBI, lung contusion, etc...) and interventions (surgery, transfusion) that lead to some common disease processes. #VTA23
These common disease processes include TRALI, ARDS, TIC and many more.
Of concern, ARDS is not uncommon in trauma patients.
#VTA23
Of concern, ARDS is not uncommon in trauma patients.
#VTA23
Next up are two of the Occupational Therapists from CHBAH - Marche van der Heyden and Tiffany Fairbairn - speaking on 'Sensory Stimulation in Critical Care'.
#VTA23 #critcare #FOAMcc
#VTA23 #critcare #FOAMcc
Sensory stimulation is emerging in critical care as a modality to re-establish normal functioning. Our senses are our connection to the world. There are 8 (not 5!) senses - auditory, olfactory, gustatory, visual, tactile/touch, vestibular, proprioception and interoception. #VTA23
The lesser known of these - vestibular, proprioception and interoception - all are key in self-soothing...
Interoception is the sense how different parts of our 'deep' body are feeling. There are a few activities that include all 8 senses - for example eating.
#VTA23
Interoception is the sense how different parts of our 'deep' body are feeling. There are a few activities that include all 8 senses - for example eating.
#VTA23
Midmorning #VTA23 session starting - lots of short talks so expect quick changes in topic! #critcare #FOAMcc
PARDIE stands for Pediatric ARDS Incidence and Epidemiology study. This study is one of the results of the PALISI Conference Group.
doi.org/10.1016/S2213-…
#VTA23
doi.org/10.1016/S2213-…
#VTA23
Last up for the morning session is John Davies, who is talking about 'Mechanical Ventilation during ECMO: all, some or none'.
#VTA23 #FOAMcc #critcare
#VTA23 #FOAMcc #critcare
Essential to remember the components of lung protective ventilation - tidal volume, plateau pressure, respiratory rate, PEEP, FiO2.
#VTA23
#VTA23
Do the rules of LPV change when the patient is on ECMO.
There is little doubt that (in appropriately selected patients) ECMO has a mortality benefit. Have a look at the CESAR and EOLIA trials:
doi.org/10.1016/S0140-…
doi.org/10.1056/NEJMoa…
#VTA23
There is little doubt that (in appropriately selected patients) ECMO has a mortality benefit. Have a look at the CESAR and EOLIA trials:
doi.org/10.1016/S0140-…
doi.org/10.1056/NEJMoa…
#VTA23
Next is Prof Ronel Roos, who will be speaking on 'Mobilisation Patients with Extracorporeal Circuits' #VTA23 #critcare #FOAMcc
There are different types of mobilisation.
There can be passive mobilisation or active/assisted exercises. Functional exercises can include standing, sitting, walking, or even a bike (in or out of bed). #VTA23
There can be passive mobilisation or active/assisted exercises. Functional exercises can include standing, sitting, walking, or even a bike (in or out of bed). #VTA23
Alot of this is about setup. Femoral vs upper body cannulisation makes a difference - femoral makes it more difficult. Securing the lines safely is essential, the tubing must be monitored and long enough. #VTA23
As soon as blood leaves the body, it comes into contact with foreign substances that initiate the clotting/coagulation process. The high surface area of the CRRT filters are usually where these processes are most likely to occur. #VTA23
Preserving filter life is very important, as the circuits are very expensive and cumbersome to replace. More importantly, time off CRRT reduces the efficacy of the RRT and puts the patient at risk. #VTA23
Prof Gavin Joynt speaking on 'Personalised Antibiotic Prescription in the Critically Ill Patient'
#VTA23 #critcare #FOAMcc
#VTA23 #critcare #FOAMcc
Antibiotics are different from fluids in that, although they are crucial in reducing mortality, their effect is not immediately apparent. The consequences of underdosing or overdosing are quite real though. #VTA23
We often worry about overdosing, but underdosing puts not only the individual patient at risk, but also other patients in (or coming to the unit) who may be exposed to the eventual MDR organisms that arise.
doi.org/10.1128/AAC.02…
#VTA23
doi.org/10.1128/AAC.02…
#VTA23
First session of Saturday's session of #VTA23 - Dr Jacqui Brown on 'Personalised Fluid Management' #critcare #FOAMcc
The first buffered IV fluids were administed during the cholera epidemic in the UK in 1832. However, fluid therapy only entered main stream medical practice around the first world war. #VTA23
However, some time has passed since then. We have entered the era of personalised on individualised fluid management. There are many paradigms that can assist with this - ROSE, 7 D's, etc...
#VTA23
#VTA23
First talk of the day - Dr Hilary Klonin, a paediatric intensivist from Hull University Teaching Hospital Trust - on 'Less is more, except when it isn't'. Talking about paediatric BP targets in critical care. #VTA23
Up to 50% of paediatric ICU survivors suffer from some sort of impairment. Could this be because the BP targets in paediatric ICU are unclear and too high a target is used? #VTA23
In 2008, a review at their hospital challenged the BP target of the 50th centile for age, and wanted to compare it to a permissive BP target. This was to be done only in critically ill patients, but started from the ED or ward, until critical illness resolved. #VTA23