Discover and read the best of Twitter Threads about #pics
Most recents (24)
It is spring and #Yerevan has started to bloom. Yerevan is suitable for walking. At every step you will meet small miracles.
#Armenia #travel #ttot #tourism #pics #Caucasus



#Armenia #travel #ttot #tourism #pics #Caucasus




Cherry trees decorate the Armenian capital Yerevan in spring. twitter.com/i/web/status/1… 

1/🧵Your brain “on COVID”🧠
Let’s integrate >20 studies on #LongCOVID neuropathology
My 24 y/o patient explained: “I don’t have a future because I can’t think anymore.”
Let’s talk:
Autopsy Studies
Viral persistence
Brain Size & Disability
Recovery & Hope
H/T pic 👁️ tw 13
Let’s integrate >20 studies on #LongCOVID neuropathology
My 24 y/o patient explained: “I don’t have a future because I can’t think anymore.”
Let’s talk:
Autopsy Studies
Viral persistence
Brain Size & Disability
Recovery & Hope
H/T pic 👁️ tw 13

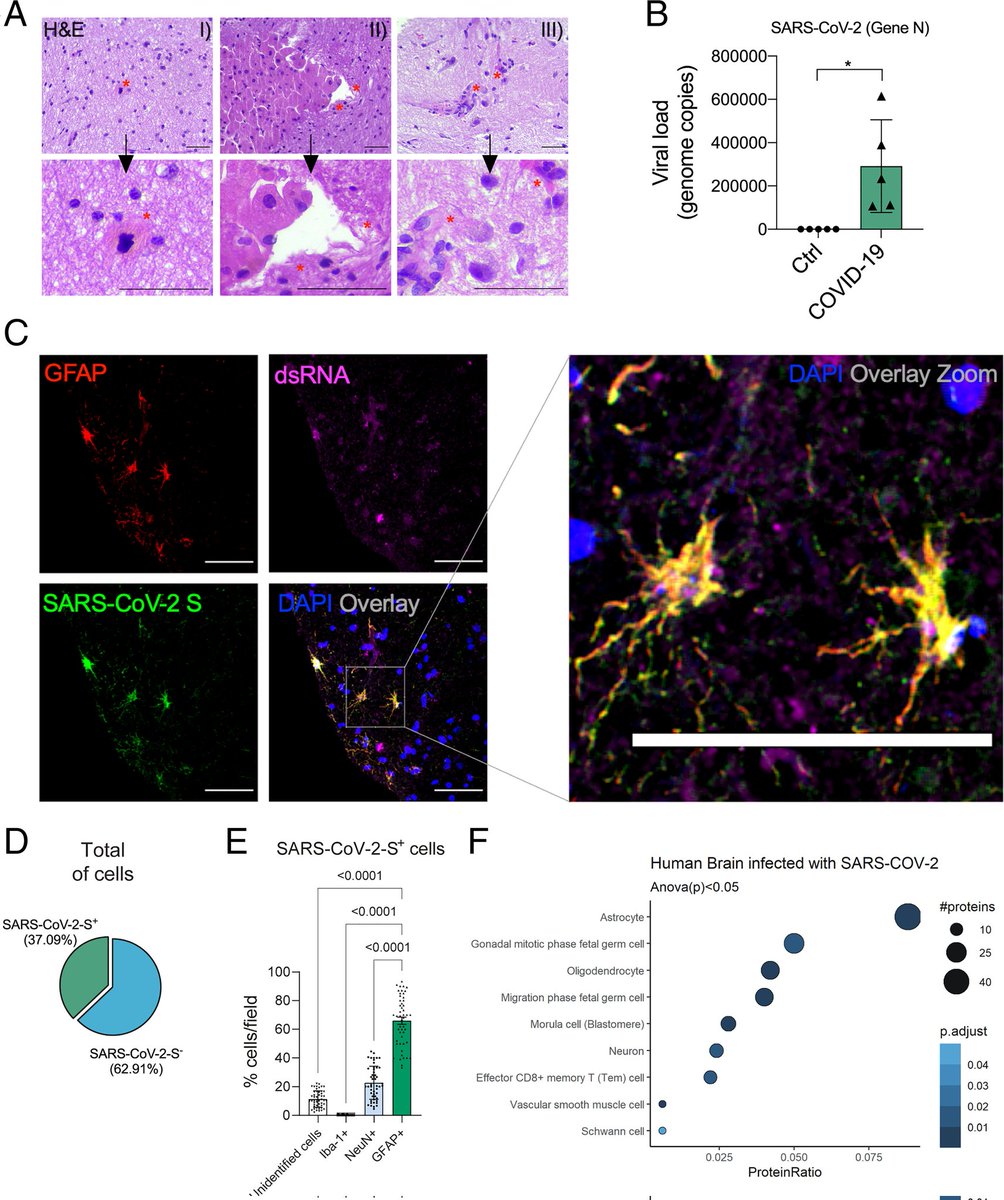
2/ Autopsy Data 🧠
Despite initial improvement from COVID, these (N=27) pts got progressively sicker & died
From their autopsies, the authors found “SARS-Cov-2 infection persisted significantly longer than suggested by standard PCR-negative tests.”
bit.ly/3JrcX3l

Despite initial improvement from COVID, these (N=27) pts got progressively sicker & died
From their autopsies, the authors found “SARS-Cov-2 infection persisted significantly longer than suggested by standard PCR-negative tests.”
bit.ly/3JrcX3l


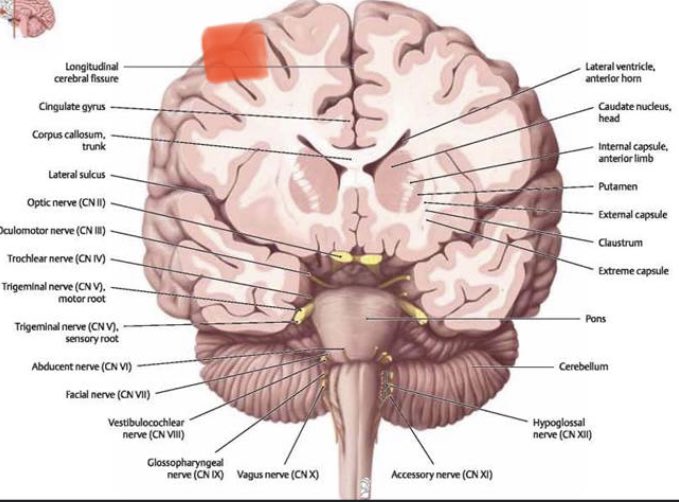
3/ Brain donation from 1st wave COVID patients (N=9) shows widespread endothelial activation, microclots & platelet aggregation supporting COVID as a vascular disease that yields real brain pathology.
IMAGE👇shows microglial nodules & neuronal injury
bit.ly/3kVCW8M


IMAGE👇shows microglial nodules & neuronal injury
bit.ly/3kVCW8M



🧵We often refer our patients for "neuropsychological" testing but what exactly is it, do you need it, and how does it add value? A thread. 1/10 @CIBScenter
Neuropsychological testing - also known as cognitive testing - aims to provide a comprehensive look at key areas of your cognitive functioning - aspects of your memory, attention, processing speed, executive functioning and more. It is a "deep dive." 2/10
Neuropsychological testing contrasts with cognitive screening (CS). Often 5 or 10 or so minutes in length. CS has a valuable place and a role to play but it provides a brief glimpse, has limitations especially in mild cases, and is not diagnostic. @CIBScenter 3/10
🧵We've been leading support groups for #ICU survivors for nearly 10 years (over 2 years with #LongCovid patients). Across literally thousands of patient encounters, what have we learned? I'll unpack these insights in tweets to follow. Thanks for reading them. @CIBScenter 1/10
To begin, the ROI for support groups is enormous- they require minimal expenses, utilize few resources, allow you to touch the lives of sometimes dozens of people at the same time, and contribute to changed lives. An inexpensive way to make a big impact. 2/10
They require competent leaders who understand group processes. You can find such people or you can become one but make sure that for at least one group leader, this is not their "first rodeo." We don't all have to be experts but we owe members that much. 3/10
Executive dysfunction is common in survivors of #Covid_19 and #PICS but how is it expressed? Let's unpack the expressions of this condition in a 🧵. @CIBScenter @WesElyMD 1 of 5 

The 'sine qua non' of executive functioning is planning. Often measured using the WCST or the Tower Test. Deficts reflect an inability to formulate strategies, to take efficient routes, to anticipate needs in advance, to tackle problems systematically. @CIBScenter
Another key component is called "set shifting" - assessed on brief cognitive tests like the Trails B Test - it involves the ability to transition rapidly from one type of task to another, and then back again. Set shifting deficits interfere at home and work. @CIBScenter
Whether the brain is damaged from a hit to the head like w/ concussion or damaged from a viral or bacterial infection, the edema/inflammation can cause strikingly similar symptom presentation in many patients, eg sensory overload/intense focus causing nausea + vomiting #LongCOVID
From the beginning of the pandemic it’s something that has stood out from patient reports. High functioning people saying they can’t read. That sound, light, movement *hurts* them now. That they need to take cognitive breaks or very slow processing. #pwME #LongCOVID #PICS #Lyme
And I learned how poorly we actually care for patients after concussion. How very little we have to offer them from a medical perspective, especially those whose symptoms linger.
As we learn more about the various ways the brain can be damaged, I hope we find better ways to heal
As we learn more about the various ways the brain can be damaged, I hope we find better ways to heal
Whether you look for #casual fling,or hot talk,or want to do some window #shopping with a chance of a naughty affair online,here is your one-stop solution.
Check this simple , no BS site which posts info on best latest hookup websites,mostly free ones.
Check this simple , no BS site which posts info on best latest hookup websites,mostly free ones.
The idea is to give you more time for actual hookups instead of browsing through tons of garbage and often fake #dating websites and apps. 

Just click on any of the #pics or buttons on this #site and you won't be disappointed!
Here you go:
👇👇👇
localhookups.best
Here you go:
👇👇👇
localhookups.best
1/🧵Our speed in understanding Long COVID is accelerating‼️
Here I cover a smorgasbord of recent COVID data on…
📍Brain Aging
📍Genetics
📍Epidemiology
📍PEM
📍Self-Protection
Knowledge is Power.
We are all at risk of losing Brain Power from #LongCOVID.
Let’s learn…
Here I cover a smorgasbord of recent COVID data on…
📍Brain Aging
📍Genetics
📍Epidemiology
📍PEM
📍Self-Protection
Knowledge is Power.
We are all at risk of losing Brain Power from #LongCOVID.
Let’s learn…
2/ COVID ages our brains 😫
Cognitive decline is part of growing old, but this is scary.
Hot new data w age-matched uninfected control ICU patients show how COVID is associated w Molecular Signatures of an Aging Brain.
See Fig 2 a/b/c BELOW
go.nature.com/3UHvyKh

Cognitive decline is part of growing old, but this is scary.
Hot new data w age-matched uninfected control ICU patients show how COVID is associated w Molecular Signatures of an Aging Brain.
See Fig 2 a/b/c BELOW
go.nature.com/3UHvyKh


3/ Genetics
This study included normal controls. Gene expression changes occur during acute COVID19 in hospital that are associated w subsequent LongCOVID.
This was especially seen in antibody producing Plasma Cells, which explained symptom clusters.
go.nature.com/3FMcois



This study included normal controls. Gene expression changes occur during acute COVID19 in hospital that are associated w subsequent LongCOVID.
This was especially seen in antibody producing Plasma Cells, which explained symptom clusters.
go.nature.com/3FMcois




1/🧵 Micro Clots & Endothelial Dysfunction in Long COVID
Plus new Epidemiology in @JAMA_current some say proves #LongCOVID is a hoax⁉️
Truth is…endothelial dysfunction plus inflammation can lead to life-altering brain & body dz.
Let’s explore data
Pic H/T @VirusesImmunity
Plus new Epidemiology in @JAMA_current some say proves #LongCOVID is a hoax⁉️
Truth is…endothelial dysfunction plus inflammation can lead to life-altering brain & body dz.
Let’s explore data
Pic H/T @VirusesImmunity

2/ Remember that Vascular flow problems don’t occur in isolation from inflammation.
This new piece by @Jamie_Ducharme balances the discussion well.
It’s time for great studies & NOT immediate widespread treatment with blood thinners that might harm.
bit.ly/3He2FCj
This new piece by @Jamie_Ducharme balances the discussion well.
It’s time for great studies & NOT immediate widespread treatment with blood thinners that might harm.
bit.ly/3He2FCj
3/ The urgency is that people are living w what amounts to newly acquired #dementia.
This WaPo piece starts w “Haze. Slow. Drunk. Lost.”
Our patients are adamant that descriptors like #fatigue & #brainfog don’t do justice to what makes them suicidal.
wapo.st/3YbRJLQ
This WaPo piece starts w “Haze. Slow. Drunk. Lost.”
Our patients are adamant that descriptors like #fatigue & #brainfog don’t do justice to what makes them suicidal.
wapo.st/3YbRJLQ
1/🧵🎥 How do “Dominoes of life” fall in critical illness⁉️
A pt arrives awake & talking but vomiting. In just 8 hrs he nearly dies of sepsis 🤯
Lung & kidney failure, heart attack, coma.
How can this happen & can we save him?
This🧵can help us understand the “arc of illness”
A pt arrives awake & talking but vomiting. In just 8 hrs he nearly dies of sepsis 🤯
Lung & kidney failure, heart attack, coma.
How can this happen & can we save him?
This🧵can help us understand the “arc of illness”
🔴Cuánto tiempo covid remodela el cerebro y cómo podemos tratarlo
La buena noticia es que, al menos en algunos pacientes, los efectos prolongados de covid en el cerebro pueden no ser permanentes o progresivos.
Perspectiva de @WesElyMD
🧶🪡Mega-Hilo en Español, por favor RT
La buena noticia es que, al menos en algunos pacientes, los efectos prolongados de covid en el cerebro pueden no ser permanentes o progresivos.
Perspectiva de @WesElyMD
🧶🪡Mega-Hilo en Español, por favor RT
Está es la inquietante ciencia cerebral del COVID prolongado 🧠
📍Reducción del cerebro 📍Fantasmas Coronavirus
📍Autoinmunidad
📍Grupos clínicos
@washingtonpost
wapo.st/3wvPBlF
📍Reducción del cerebro 📍Fantasmas Coronavirus
📍Autoinmunidad
📍Grupos clínicos
@washingtonpost
wapo.st/3wvPBlF
1/🧵 The Haunting Brain Science of Long COVID 🧠
@washingtonpost Aug 25
📍Brain shrinking
📍Corona ghosts
📍Autoimmunity
📍Clinical clusters
“The good news is that in some pts #LongCovid #BrainFog may not be permanent.”
Link👇 but paywall so see 🧵
wapo.st/3wvPBlF

@washingtonpost Aug 25
📍Brain shrinking
📍Corona ghosts
📍Autoimmunity
📍Clinical clusters
“The good news is that in some pts #LongCovid #BrainFog may not be permanent.”
Link👇 but paywall so see 🧵
wapo.st/3wvPBlF

2/ Mild Covid is biologically dangerous long after initial viral infection.
81 mild COVID pts:
Study revealed:
✔️Astrocytes (🧠 support cells for neurons) get infected
✔️Neurotransmitters are altered
✔️Neurons die indirectly
✔️Then we lose brain power
bit.ly/3pcqbFV

81 mild COVID pts:
Study revealed:
✔️Astrocytes (🧠 support cells for neurons) get infected
✔️Neurotransmitters are altered
✔️Neurons die indirectly
✔️Then we lose brain power
bit.ly/3pcqbFV

3/ Epidemiology💥
Long COVID is tightening its grip on society.
We’re still losing >600 people a day to death from COVID in US alone
Over 100,000 new infections per day (Johns Hopkins data).
This is an epic global 🌍#PublicHealth catastrophe.
wb.md/3SKjGrh
Long COVID is tightening its grip on society.
We’re still losing >600 people a day to death from COVID in US alone
Over 100,000 new infections per day (Johns Hopkins data).
This is an epic global 🌍#PublicHealth catastrophe.
wb.md/3SKjGrh
1/🧵 An exacerbating factor in #LongCOVID is the “Quality of Life (QOL) Gap”🧵👇
…when a person’s expectations about QOL are at odds w their reality.
“Covid was over & Long COVID hit my brain, heart & GI.”
Let me unpack a study of ICU survivors…
bit.ly/3vp0AMl
…when a person’s expectations about QOL are at odds w their reality.
“Covid was over & Long COVID hit my brain, heart & GI.”
Let me unpack a study of ICU survivors…
bit.ly/3vp0AMl

2/ Read the thread I attached to the first tweet.
From the cancer literature, we learned about the QOL Gap.
If people appropriately prepare for their “ACTUAL” QOL, there’s a narrow gap and all is well.
If not, #Depression & #Despair too often set in.
From the cancer literature, we learned about the QOL Gap.
If people appropriately prepare for their “ACTUAL” QOL, there’s a narrow gap and all is well.
If not, #Depression & #Despair too often set in.
3/ This study from Johns Hopkins by @vitaincerta & team adds to our understanding in a way that will apply so well to #COVID ICU survivors.
These are ARDS patients, which is almost always what lands COVID pts in the ICU and later with #PICS.
@ChestCritCare
These are ARDS patients, which is almost always what lands COVID pts in the ICU and later with #PICS.
@ChestCritCare

🧵1/ Here’s your “Big Picture” of COVID & Long COVID for 2022
See my new Figure👇 summarizing #COVID19 Management & Outcomes
Two years in & we have splendid choices.
Stay in peaceful waters of prevention (green) or risk treacherous cliffs of #LongCOVID & Death (red & black)…
See my new Figure👇 summarizing #COVID19 Management & Outcomes
Two years in & we have splendid choices.
Stay in peaceful waters of prevention (green) or risk treacherous cliffs of #LongCOVID & Death (red & black)…

2/ Knowledge is Power, and our knowledge has grown dramatically.
Let’s take a look at where we were just 2 years ago - even though it seems like 20 yrs ago.
April 2020: our approach & understanding of COVID looked like this👇.
We didn’t even know about #LongCOVID yet 🤯
Let’s take a look at where we were just 2 years ago - even though it seems like 20 yrs ago.
April 2020: our approach & understanding of COVID looked like this👇.
We didn’t even know about #LongCOVID yet 🤯

3/ Remember, with #LongCOVID, your brain & heart are at stake.
@JohnsHopkinsSPH reports on emerging data: “COVID doesn’t discriminate when it comes to heart problems.”
Anyone affected may develop clots, arrhythmias & strokes >1 yr later.
Link &🧵below
bit.ly/3KzYcbp
@JohnsHopkinsSPH reports on emerging data: “COVID doesn’t discriminate when it comes to heart problems.”
Anyone affected may develop clots, arrhythmias & strokes >1 yr later.
Link &🧵below
bit.ly/3KzYcbp
Ok. As promised, here is a super-🧵 on cognition and #LongCovid. This will be a combination of published material and things that we have observed in-clinic. This is not intended to be definitive nor epidemiological and so it is highly likely that your personal experience (1/n)
may deviate significantly. This is about my reading and experience of cognition and #LongCovid but from what I have seen shared in the comments of my tweet yesterday, it seems that much of this may apply to other infection-associated chronic illnesses (h/t @microbeminded2) (2/n)
such as #MECFS, #Lyme and #dysautonomia/#POTS to name a few. Let’s start out with naming. I try not to use the term “brain fog” because I don’t think it conveys the seriousness. People with LC are experiencing cognitive dysfunction that often results in cognitive impairment (3/n)
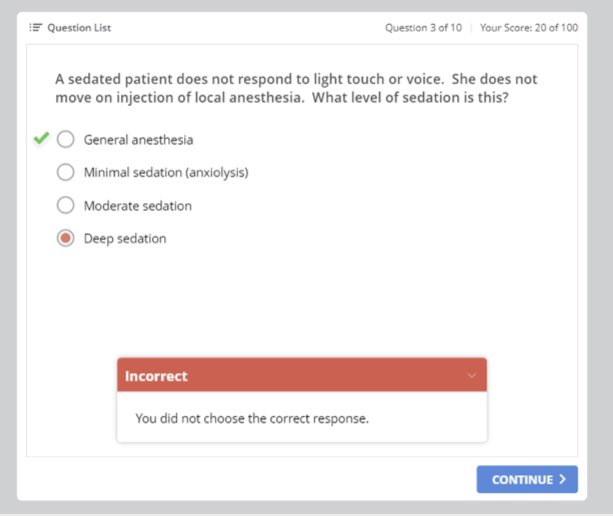
1/🧵 You have a COVID ICU patient on benzos who doesn’t respond to needle injection of local anesthetic do to sedatives.
What depth of sedation do you consider this? (it was a CME question just now)
What depth of sedation do you consider this? (it was a CME question just now)
1/🧵🎥 “It’s a very bad disease. It can be overcome.”
My #COVID patient tearfully speaks of his BIG DECISION on the ventilator.
This soldier & leukemia survivor made it through 3 weeks on a ventilator. How?
Video shown w his permission “to help others find hope, Doc.”
#Hope
My #COVID patient tearfully speaks of his BIG DECISION on the ventilator.
This soldier & leukemia survivor made it through 3 weeks on a ventilator. How?
Video shown w his permission “to help others find hope, Doc.”
#Hope
1/🧵 Why is COVID hospitalization like 2X sticks of dynamite 🧨?
A thread on the ICU portion… #PICS + #LongCOVID.
Prevent this w 3 steps:
📌Avoid #COVID by Vax & Mask
📌Avoid severe COVID by Paxlovid & Monoclonal Ab
📌👇 read here about PICS & how to reduce injury in the ICU
A thread on the ICU portion… #PICS + #LongCOVID.
Prevent this w 3 steps:
📌Avoid #COVID by Vax & Mask
📌Avoid severe COVID by Paxlovid & Monoclonal Ab
📌👇 read here about PICS & how to reduce injury in the ICU
2/ Here’s what you must know if you get too sick & land in an ICU.
History Lesson 📝
In the past, too many decisions in #CriticalCare were guided by fear. We oversedated patients for too long out of worry they might self-extubate & pull off restraints.
That’s happening again 🤮
History Lesson 📝
In the past, too many decisions in #CriticalCare were guided by fear. We oversedated patients for too long out of worry they might self-extubate & pull off restraints.
That’s happening again 🤮

1/🧵 Seeing Differently in #COVID ICU Care 👁
The world tells me “stuff” & “freedom ” bring happiness, yet neither suffice or satisfy.
If I reject chances to serve my suffering patients, I am left bereft.
Merciful care brings healing & provides joy all around.
What is #Mercy?
The world tells me “stuff” & “freedom ” bring happiness, yet neither suffice or satisfy.
If I reject chances to serve my suffering patients, I am left bereft.
Merciful care brings healing & provides joy all around.
What is #Mercy?

2/ My working definition of mercy is my willingness to dive into the chaos of another person’s life & provide lifting & healing.
Often as an ICU physician I do the former but not the latter.
That is, I dive into their #chaos without admitting I don’t know what’s right for them.
Often as an ICU physician I do the former but not the latter.
That is, I dive into their #chaos without admitting I don’t know what’s right for them.

3/…but without performing actions that lead to lifting and healing of my patient’s spirit & mind, what I’m doing is dispensing false mercy.
eg, If in #COVID, I make the lungs 🫁 my whole goal, sedate & depersonalize someone for too long, I beget new diseases.
#PICS #LongCovid
eg, If in #COVID, I make the lungs 🫁 my whole goal, sedate & depersonalize someone for too long, I beget new diseases.
#PICS #LongCovid

1/🧵 How do #COVID patients suffer after the ICU?
This new @JAMA_current study of 246 Dutch pts shows that 3 out of 4 people had physical problems 1 YEAR LATER plus 1 in 4 have #brainfog, depression & anxiety.
What do we call this?
#LongCOVID #PICS
bit.ly/3o4djkT
This new @JAMA_current study of 246 Dutch pts shows that 3 out of 4 people had physical problems 1 YEAR LATER plus 1 in 4 have #brainfog, depression & anxiety.
What do we call this?
#LongCOVID #PICS
bit.ly/3o4djkT

2/ The paper is also discussed in @Medscape👇: “Our study shows what an impact ICU admission has on former #COVID19 pts. Even after 1 year, half are tired or experience lack of the energy to fully resume their work," says author Marieke Zegers, PhD
wb.md/33U9DeF
wb.md/33U9DeF
3/ I searched this paper for well-known terms like post-intensive care syndrome #PICS, #LongCOVID & even “post-acute sequelae of COVID”#PASC
NADA. Zip. Zilch.
Why weren’t these names mentioned? At the very least, these pts’ disabilities are DEFINITELY PICS & underestimated btw
NADA. Zip. Zilch.
Why weren’t these names mentioned? At the very least, these pts’ disabilities are DEFINITELY PICS & underestimated btw
1/🧵Important = Brain Injury in #COVID💥
📍N=251 hospitalized COVID pts had biomarkers of neurodegeneration (dying brain cells).
📍Previously healthy COVID pts had ⬆️er levels than Alzheimer’s pts!
How do we understand this?
Hint: #Vaccinate yourself
bit.ly/3frTcbB


📍N=251 hospitalized COVID pts had biomarkers of neurodegeneration (dying brain cells).
📍Previously healthy COVID pts had ⬆️er levels than Alzheimer’s pts!
How do we understand this?
Hint: #Vaccinate yourself
bit.ly/3frTcbB



2/ These elevated brain biomarkers indicate disease to different types of brain cells (eg, astrocytes, glial cells, neurons) in COVID patients. These were early unvaccinated pandemic patients. Vaccinated people will be less prone. WHY?
3/ There isn’t a ton of brain invasion by COVID. We think most of the 🧠 injury is INDIRECT. Meaning downstream injury from 1. upstream inflammation 2. blood clotting & 3. heavy sedation causing #delirium, which we proved to be a #dementia risk factor!
bit.ly/3qCaOrQ
bit.ly/3qCaOrQ
1/🧵🎥 A young mom suffering #COVID. Her husband is scared.
We need to prevent serious long-term complications. Her new normal will likely include PTSD, Dementia, Depression & severe physical disability. (shown w Perm)
Not so “mild” ➡️ Do you want this?
#vaccinate
#LongCOVID
We need to prevent serious long-term complications. Her new normal will likely include PTSD, Dementia, Depression & severe physical disability. (shown w Perm)
Not so “mild” ➡️ Do you want this?
#vaccinate
#LongCOVID
2/ what you need to know about ICUs, #PICS and #LongCOVID prevention:
I wrote this @thedailybeast piece👇 to help empower you as patients & families. It’ll tell you what you need to know & ask your team for amid the chaos and confusion.
There’s more…
bit.ly/3DhC6Xe
I wrote this @thedailybeast piece👇 to help empower you as patients & families. It’ll tell you what you need to know & ask your team for amid the chaos and confusion.
There’s more…
bit.ly/3DhC6Xe
3/ This patient on 100% O2 and high-dose propofol & fentanyl did not need both agents. When able, we try to avoid prop & benzos. We stopped Prop, continued Fentanyl & added dexmedetomidine because it’s shorter acting & won’t build up so much in her brain.
This is the #A2Fbundle.
This is the #A2Fbundle.
1/🧵 Brain + Body damage in #COVID & Critical Illness
Sepsis -bacterial, viral, fungal- can cause rapid-onset #dementia. Finishing this test should be easy at her age but Millions of brain cells are damaged!
Protect yourself & others: #Vaxx + #Mask
H/T @trishla_17 for helping
Sepsis -bacterial, viral, fungal- can cause rapid-onset #dementia. Finishing this test should be easy at her age but Millions of brain cells are damaged!
Protect yourself & others: #Vaxx + #Mask
H/T @trishla_17 for helping
2/ Our brain depends on a delicate balance of blood flow, nutrients & oxygen. When someone gets critically ill w #Covid or from other causes, that balance is dramatically disrupted. Small blood clots, dropping oxygen levels cause 🧠 damage.
bit.ly/36K5F65
bit.ly/36K5F65
3/ It’s odd to me that people don’t see severe COVID as a form of VIRAL SEPSIS. Sepsis is when infection of any kind causes your organs to begin to fail – lungs, brain, heart, kidneys. It’s EXACTLY what we see day-in day-out in the COVID ICU.
bit.ly/3eM8pUx
bit.ly/3eM8pUx

1/🧵For months I’ve been grappling with what seemed like a real gap in conversations about #LongCOVID.
Here in @STATnews, I introduce you to 30 references & 3 #COVID survivors – Ray, Pam, and Carolyn – who taught me a lot. I hope you think so, too…
bit.ly/2Zb9S2J
Here in @STATnews, I introduce you to 30 references & 3 #COVID survivors – Ray, Pam, and Carolyn – who taught me a lot. I hope you think so, too…
bit.ly/2Zb9S2J
2/ "I feel like I'm getting the silent treatment & it's killing me," #LongCOVID pt Pamela Bishop confided in me about her months-long interactions as she tried to get answers about a strange array of symptoms that have plagued her since recovering from #Covid19.
Pam then & now…
Pam then & now…

3/ Up to1 in 3 COVID survivors report experiencing #longCovid symptoms 3 to 6 months later. Their stories give me an extreme case of déjà vu because this is playing out similarly to the problem of long-term survivorship after non-COVID critical illness.
bit.ly/3vzcIdn
bit.ly/3vzcIdn