#CALCIPHYLAXIS!
This is a devastating diagnosis often seen in inpatients, so this goes to all the @DermHospitalist & #hospitalists out there!
#FOAMed #MedEd #dermatology #dermatologia #dermtwitter #medtwitter @SHMlive @DermHospitalist
1/
2/
Yes! The differential dx for this is anything that may block blood flow, mainly vasculitis and vasculopathy. So, how exactly do you make the dx?
4/
5/
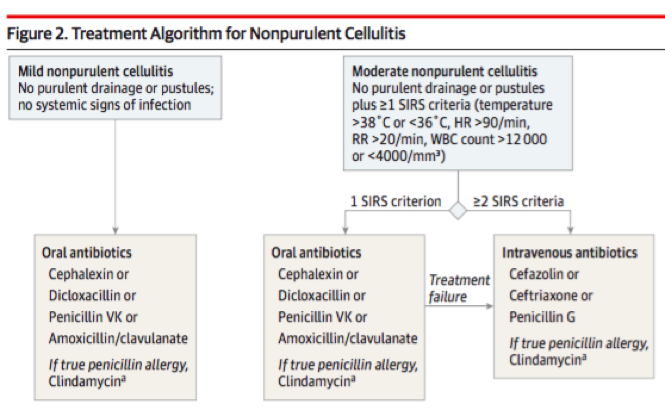
jamanetwork.com/journals/jamad…
6/
7/
8/
9/
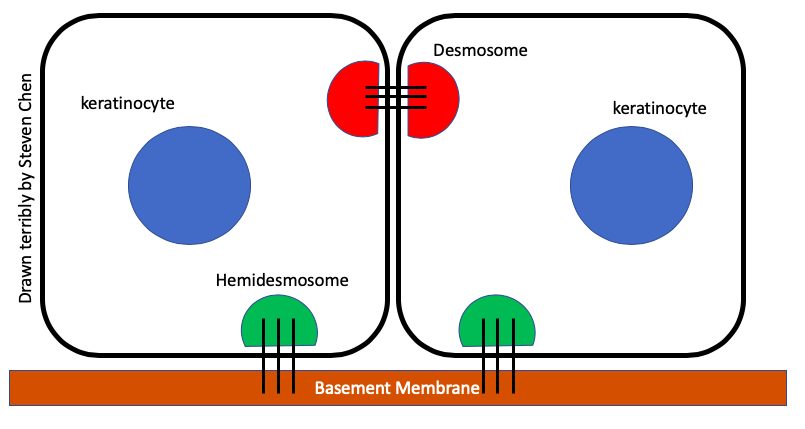
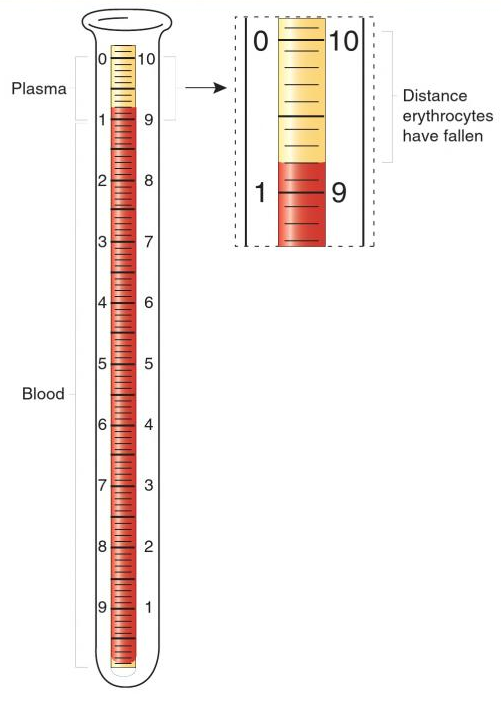
✔️Calciphylaxis is from impaired blood flow in skin arterioles +/- thrombosis
✔️It's crazy painful & terrible for patients
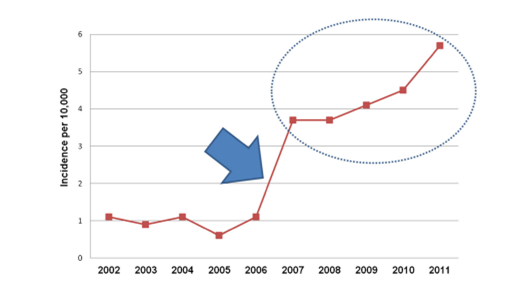
✔️Evaluation includes RFs (mainly ESRD on HD), skin bx, labs, & ruling out other causes
✔️Mortality is high, largely from sepsis
10/
PC for #3 and 10: ncbi.nlm.nih.gov/pmc/articles/P…
11/
12/
13/
jamanetwork.com/journals/jamad…
14/
15/
✔️Calciphylaxis treatments require multidisciplinary collaboration.
✔️Patients can improve, but it takes time and dedication.
✔️Vigilance for infection, excellent wound care are pillars for treatment.
✔️Involve #dermatology and #nephrology early!
16/
If you liked it, & want to discuss this field more, consider joining #dermjc and #nephjc in August for a joint discussion on calciphylaxis! Would love to see more collaboration here on #medtwitter!
@DermatologyJC
17/17