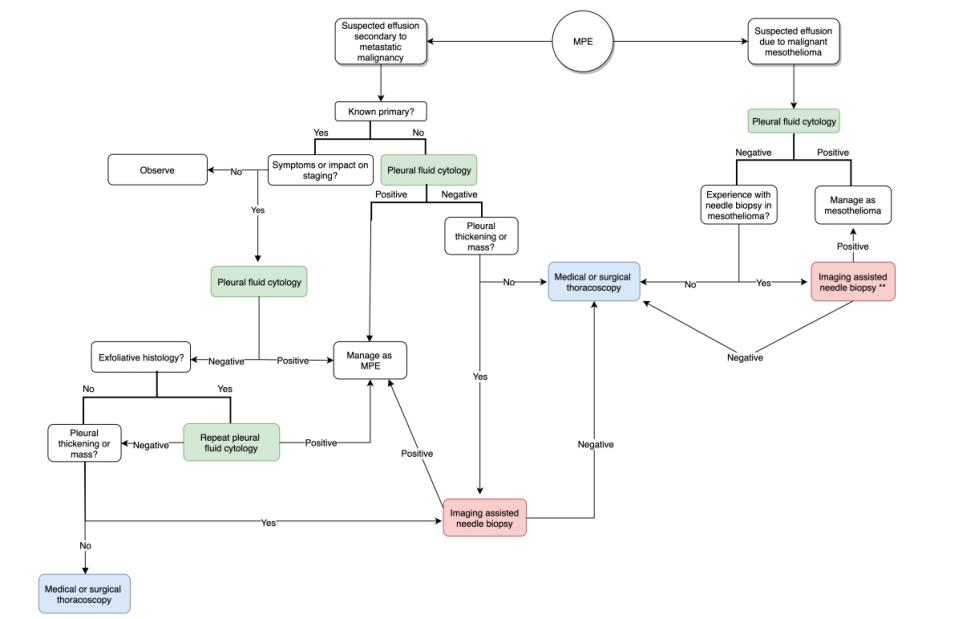
⚓️#MPE: Pl. Effusions (#pleff) w/ neoplastic cells/tissue
⚓️Paramalignant eff: related to malignancy but not due to it eg: endobronchial obstruction or PE
Why is it important to diagnose #MPE?
While you ponder, LUNG and BREAST are commonest primaries metastatic to the pleural space! PMID: 24360987
#thoracentesis + PF analysis is the next step!
#Trivia: “Cancer Ratio” = Sr. LDH / Pl. ADA >20 has sensitivity of 98% and specificity of 94% for #MPE!
📈Yields much higher for "exfoliative" cancers: Lung AdenoCa / Ovarian
👎Yields VERY low for "non-exfoliative": Squamous #LungCancer
So: repeat cyto if primary likely exfoliative, otherwise proceed to next step!
What is your practice? Leave comments!
For those of you wanting to learn more about "exfoliative" aspects of malignancies: I recd this 1964 article by Dr. Naylor from @UMich!
bit.ly/2XOIBjR
So! pleff cyto has failed you, what's next??
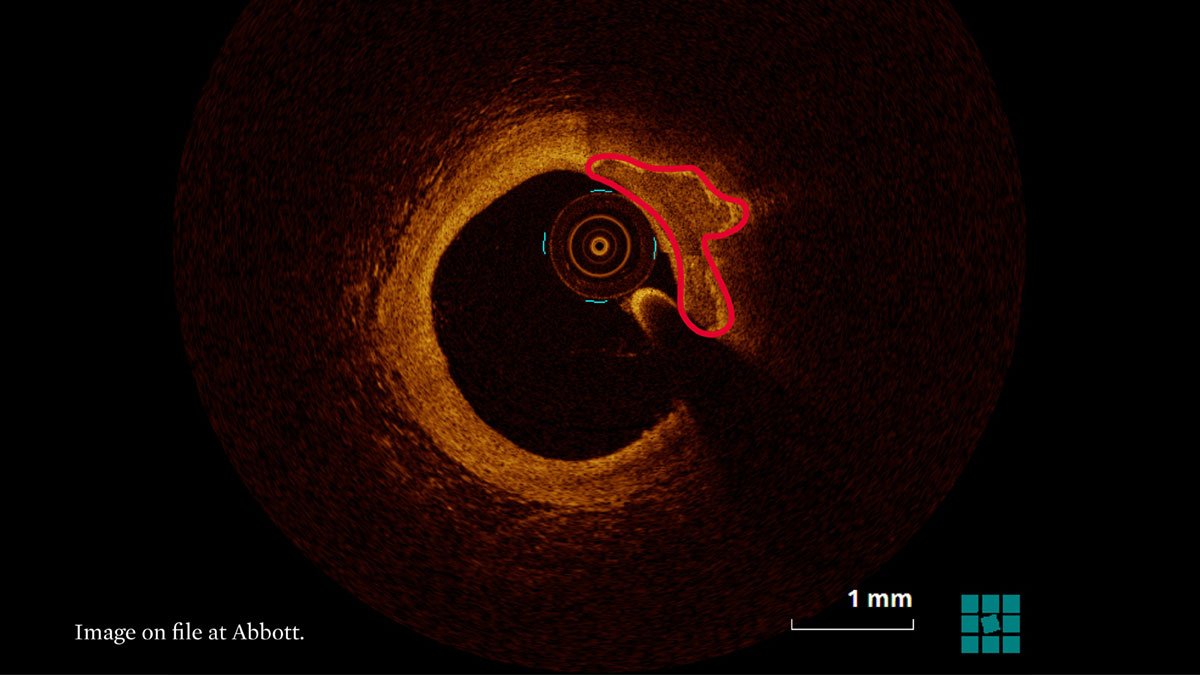
Real time CT guided or POCUS guided #pleuralbiopsy is the next choice, depending on local availability (sens high 80%)!
NOTE: Sensitivity is higher if pleura >1 cm thick!
PMID: 25997433
VATS vs Medical Thoracoscopy (#MT): Surgeon vs Pulm (usually), GA vs Local +/- TIVA
Co-author @naj_rahman (PMID: 20696694): Very low mortality for #MT
Recent data (PMID:29577922) for VATS also shows improved risk profile!
Not every patient is capable of undergoing thoracoscopy, esp the GA and single lung ventilation need for VATS!
Some absolute contraind for #thoracoscopy:
🛑Lung extensively adherent to chest wall
🛑Resting hypercapnia, likely to worsen during/after procedure
Upto 30% cytology and histology negative pleural effusions are not diagnosed and get labeled "non specific pleuritis".
Upto 12% OF THESE EVENTUALLY TURN OUT TO BE PLEURAL MALIGNANCY, SO PLEASE BE CLINICALLY VIGILANT W/ THESE PATIENTS!
(PMID: 27625443)
In summary:
- Send 75 cc for cyto, 150 cc for cell block
- Repeat cyto for exfoliative types
- Proceed to imaging Bx or thoracoscopy per risk profile and local exp
- Stay vigilant if no diagnosis!
Finally, thank you @GoodishIntent @ETSshow @laxswamy @hshanawaniMD for always encouraging me to be a better teacher!