Discover and read the best of Twitter Threads about #clinicalpearls
Most recents (24)
Weekend Digest
Name the Pathogen
Five Clues
1. Tumbling #GPB
2. #Pregnancy
3. #Delicatessen
4. #Meningoencephalitis
5. #Ampicillin + #gentamicin
Name the Pathogen
Five Clues
1. Tumbling #GPB
2. #Pregnancy
3. #Delicatessen
4. #Meningoencephalitis
5. #Ampicillin + #gentamicin

#Listeria monocytogenes
High-risk foods: unpasteurized cheeses, hot dogs and deli/lunchmeats.
High-risk groups:
- pregnant women
- newborns
- older adults
- people with weakened immune systems
High-risk foods: unpasteurized cheeses, hot dogs and deli/lunchmeats.
High-risk groups:
- pregnant women
- newborns
- older adults
- people with weakened immune systems
#Listeriosis in pregnancy
1. Febrile gastroenteritis
2. Bacteremia
3. CNS infection uncommon
Most common in 3rd trimester
Listeria can cross placental barrier —> fetal death, premature birth, infected newborn
Granulomatosis infantiseptica
eurosurveillance.org/content/10.280…
1. Febrile gastroenteritis
2. Bacteremia
3. CNS infection uncommon
Most common in 3rd trimester
Listeria can cross placental barrier —> fetal death, premature birth, infected newborn
Granulomatosis infantiseptica
eurosurveillance.org/content/10.280…
Weekend Digest
Name the Pathogen
Five Clues
1. Gram-positive bacillus with tumbling motility
2. Food safety
3. Age, pregnancy and steroids
4. Rhombencephalitis
5. Ampicillin+Gentamicin
Name the Pathogen
Five Clues
1. Gram-positive bacillus with tumbling motility
2. Food safety
3. Age, pregnancy and steroids
4. Rhombencephalitis
5. Ampicillin+Gentamicin

2/
#Listeria monocytogenes
Soil
Decaying plant matter
Processed/unprocessed food (deli meats, hotdog, soft cheese, pate, fruits, greens/salads)
Oral route —> intestinal mucosa penetration —> systemic infection
#Listeria monocytogenes
Soil
Decaying plant matter
Processed/unprocessed food (deli meats, hotdog, soft cheese, pate, fruits, greens/salads)
Oral route —> intestinal mucosa penetration —> systemic infection
3/
#Listeria monocytogenes and food safety!
Listeria survives in refrigeration temperature
Sporadic isolated cases
Occasional outbreaks due to food contamination (see link for recent outbreak)
fda.gov/food/outbreaks…
#Listeria monocytogenes and food safety!
Listeria survives in refrigeration temperature
Sporadic isolated cases
Occasional outbreaks due to food contamination (see link for recent outbreak)
fda.gov/food/outbreaks…
#Cefalea Puntos claves: anamnesis y examen clínico inicial.
∙ Evaluar gravedad: puede ir desde leve a alta intensidad (“la más grave de la vida del paciente”). Este último grado de intensidad puede apreciarse en cefalea tipo “trueno” u otros tipos de cefalea de altísima intensidad y brusca aparición y necesita atención prioritaria.
∙ Antecedentes: hay que hacer énfasis en el estado de inmunosupresión del paciente, especialmente en presencia de cáncer o infección por virus de inmunodeficiencia humana (VIH).
#SíndromePulmónRiñón: Ayudas diagnósticas
Radiología: infiltrados con patrón alveolar de distribución simétrica, predominio central y en bases pulmonares; sin embargo, hay casos en los que los hallazgos pueden ser focales – unilaterales y discernir con otras entidades puede ser difícil.
Gasimetría arterial: hipoxemia (PaO2 menor de 60mmHg); el mecanismo de esta condición es secundaria a “shunt” y alteración de la difusión, lo que explica la pobre respuesta al oxígeno a alto flujo en la mayoría de los casos.
Time for some #SpacedRepetition from @CPSolvers @DxRxEdu @rabihmgeha
Some chat recap #ClinicalPearls and bonus pearls from #VirtualMorningReport on Friday Sept 25th clinicalproblemsolving.com/morning-report…
Case by the brilliant @Rafameed
Some chat recap #ClinicalPearls and bonus pearls from #VirtualMorningReport on Friday Sept 25th clinicalproblemsolving.com/morning-report…
Case by the brilliant @Rafameed

A 31-year-old M born and raised in Brazil w/ no PMH presented with a 3 mon history of worsening DOE, orthopnea, 7kg weight loss, abdominal distention, dry cough, and syncope
Base rate of disease for an ID case with @k_vaishnani and @Rafameed is very high
Base rate of disease for an ID case with @k_vaishnani and @Rafameed is very high
An interesting fact from @3owllearning : Depending on the clinical problems, the studies of disease probability for differential diagnosis often show 10 - 25% of cases are unexplained, even after careful examination and testing.
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha @dminter89
Chat recap of the #ClinicalPearls #VirtualMorningReport
Episode 140 - Virtual Morning Report - September 11, 2020 clinicalproblemsolving.com/morning-report…
Chat recap of the #ClinicalPearls #VirtualMorningReport
Episode 140 - Virtual Morning Report - September 11, 2020 clinicalproblemsolving.com/morning-report…

Let's start with an initial PR:
A 27 y/o male with no PMH from Mexico presents with 10 days of generalized abd pain, vomiting, diarrhea, fever, & yellowing of his eyes
Deploy our Jaundice Schema; clinicalproblemsolving.com/dx-schema-jaun…
A 27 y/o male with no PMH from Mexico presents with 10 days of generalized abd pain, vomiting, diarrhea, fever, & yellowing of his eyes
Deploy our Jaundice Schema; clinicalproblemsolving.com/dx-schema-jaun…
Other causes of yellow skin, e.g. excess beta carotene, usually do not cause deposition in conjunctiva or sclera, so eyes aren’t yellow
sounds biliary in nature, but could also consider hemolysis with gallstones like in her spherocytosis or something like that.
sounds biliary in nature, but could also consider hemolysis with gallstones like in her spherocytosis or something like that.
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
September 1st Ep. 132: clinicalproblemsolving.com/morning-report…
w/@AaronLBerkowitz @medrants @G_Khafaji @MariaMjaleman
Teaching points illustration by @sukritibanthiya
Chat recap of the #ClinicalPearls #VirtualMorningReport
September 1st Ep. 132: clinicalproblemsolving.com/morning-report…
w/@AaronLBerkowitz @medrants @G_Khafaji @MariaMjaleman
Teaching points illustration by @sukritibanthiya

First, let's start w/ an initial PR:
A 49 y/o F w/ a PMH of HTN, ETOH/THC abuse p/w bilateral leg weakness that started a week ago following during an admission for CAP that has since gotten worse along with urinary and fecal incontinence
A 49 y/o F w/ a PMH of HTN, ETOH/THC abuse p/w bilateral leg weakness that started a week ago following during an admission for CAP that has since gotten worse along with urinary and fecal incontinence
is it true weakness or asthenia?
If weakness is present, is it ascending/descending, any back pain, incontinence, sensory deficits?
is the weakness proximal, distal, both?
Also think vascular and myopathy causes
If weakness is present, is it ascending/descending, any back pain, incontinence, sensory deficits?
is the weakness proximal, distal, both?
Also think vascular and myopathy causes
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
August 17th Episode 119: clinicalproblemsolving.com/morning-report…
W / @MohitHarshMD @KromerHaylie & Ninand Bhat
Chat recap of the #ClinicalPearls #VirtualMorningReport
August 17th Episode 119: clinicalproblemsolving.com/morning-report…
W / @MohitHarshMD @KromerHaylie & Ninand Bhat

Let's start with an initial problem representation:
A 75 y/o M w/ a PMH of COPD, CAD, & aortic valve replacement p/w 2 weeks of dyspnea on exertion, 1 month of LE edema, 20 lb weight loss & recent onset PND and Orthopnea
A 75 y/o M w/ a PMH of COPD, CAD, & aortic valve replacement p/w 2 weeks of dyspnea on exertion, 1 month of LE edema, 20 lb weight loss & recent onset PND and Orthopnea
invoke the dyspnea pyramid (cardiac, pulmonary, anemia, metabolic) but addition of progressive edema and weight gain concerning for cardiac pathology
whenever we see dyspnea on exertion and bilateral LE edema we jump straight to CHF
whenever we see dyspnea on exertion and bilateral LE edema we jump straight to CHF
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
August 12th Episode 115: clinicalproblemsolving.com/morning-report…
w / Sonia Silinsky Krupnikova @Flower_freeland @pri_athavale
Teaching points @sukritibanthiya
Chat recap of the #ClinicalPearls #VirtualMorningReport
August 12th Episode 115: clinicalproblemsolving.com/morning-report…
w / Sonia Silinsky Krupnikova @Flower_freeland @pri_athavale
Teaching points @sukritibanthiya

Let’s start with an initial problem representation:
A 50 y/o F w/ a PMH of remote gastric bypass, anemia, MGUS & hereditary elliptocytosis p/w worsening fatigue, dyspnea on exertion, chronic chest discomfort and trouble sleeping at night
A 50 y/o F w/ a PMH of remote gastric bypass, anemia, MGUS & hereditary elliptocytosis p/w worsening fatigue, dyspnea on exertion, chronic chest discomfort and trouble sleeping at night
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
August 11th Episode 114: clinicalproblemsolving.com/morning-report…
W / @Anu08877649 Joshua Morris & @Rafameed
Teaching points illustration by @sukritibanthiya
Chat recap of the #ClinicalPearls #VirtualMorningReport
August 11th Episode 114: clinicalproblemsolving.com/morning-report…
W / @Anu08877649 Joshua Morris & @Rafameed
Teaching points illustration by @sukritibanthiya

Let’s start with an initial problem representation:
A 55 y/o M w/ no known PMH except a 30 pack-year history of tobacco abuse presents with recurrent syncope (lightheaded prodrome) over last 2 mon along w/ R shoulder pain, 15 lb weight loss for 3 months, and an occasional cough
A 55 y/o M w/ no known PMH except a 30 pack-year history of tobacco abuse presents with recurrent syncope (lightheaded prodrome) over last 2 mon along w/ R shoulder pain, 15 lb weight loss for 3 months, and an occasional cough
An initial evaluation of syncope should involve ruling out mimickers like Sz or TIA
The fact that he was lying down during the episode is concerning for cardiogenic cause like an arrhythmia
Also, an autonomic given the lightheadedness while lying in bed
clinicalproblemsolving.com/dx-schema-sync…
The fact that he was lying down during the episode is concerning for cardiogenic cause like an arrhythmia
Also, an autonomic given the lightheadedness while lying in bed
clinicalproblemsolving.com/dx-schema-sync…

Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
August 10th Episode 113: clinicalproblemsolving.com/morning-report…
w/ @kiaracamacho96 @RizwanDania & Maria Jose Vides
Teaching points illustration by Sukriti Banthiya
Chat recap of the #ClinicalPearls #VirtualMorningReport
August 10th Episode 113: clinicalproblemsolving.com/morning-report…
w/ @kiaracamacho96 @RizwanDania & Maria Jose Vides
Teaching points illustration by Sukriti Banthiya

Let's start with an initial problem representation:
A 73 y/o M w/ a pmh of DM2, depression, hypoTh, BPH presents w/ a few days of nocturia & LE pain & brought in bc he was found lying on the floor of his bathroom disoriented after experiencing dizziness, blurry vision & falling
A 73 y/o M w/ a pmh of DM2, depression, hypoTh, BPH presents w/ a few days of nocturia & LE pain & brought in bc he was found lying on the floor of his bathroom disoriented after experiencing dizziness, blurry vision & falling
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 31st Episode 105: clinicalproblemsolving.com/morning-report…
case presenter @Rafameed
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 31st Episode 105: clinicalproblemsolving.com/morning-report…
case presenter @Rafameed

Let’s start with a problem representation:
A 42 y/o M w/ no PMH presents with confusion and syncope but prior to this he noted 4 months of worsening cervical LAD and oral ulcerations along with a 5kg weightloss, cough, SOB w/ exertion & voice changes
A 42 y/o M w/ no PMH presents with confusion and syncope but prior to this he noted 4 months of worsening cervical LAD and oral ulcerations along with a 5kg weightloss, cough, SOB w/ exertion & voice changes
cervical adenopathy & oral ulcerations, hm
are these painful? mobile?
oral ulceration, makes us think fungal, sarcoid, &autoimmune as well
This could be TB (scrofula) or “king’s evil”, royal touch was believed to cure the disease until the 18th cent ncbi.nlm.nih.gov/pmc/articles/P…
are these painful? mobile?
oral ulceration, makes us think fungal, sarcoid, &autoimmune as well
This could be TB (scrofula) or “king’s evil”, royal touch was believed to cure the disease until the 18th cent ncbi.nlm.nih.gov/pmc/articles/P…
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 30th Episode 104: clinicalproblemsolving.com/morning-report…
W / @Sharminzi @ArsalanMedEd @medrachel @Flower_freeland @amrmousa96
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 30th Episode 104: clinicalproblemsolving.com/morning-report…
W / @Sharminzi @ArsalanMedEd @medrachel @Flower_freeland @amrmousa96
Let’s start with an initial problem representation:
A 30 y/o M w/ a PMH of lupus, pericarditis, HTN presents with 2 mon of dyspnea on exertion, worse w/ exertion, episodic CP while denying fevers, drenching night sweats, cough or weight loss
A 30 y/o M w/ a PMH of lupus, pericarditis, HTN presents with 2 mon of dyspnea on exertion, worse w/ exertion, episodic CP while denying fevers, drenching night sweats, cough or weight loss
Given her history of lupus, Autoimmune is again, as always, on the differential
He seems too young for CHF, but heart and lungs should be the initial focal point followed by anemia which is also unusual for a male at 30
He seems too young for CHF, but heart and lungs should be the initial focal point followed by anemia which is also unusual for a male at 30
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha @sargsyanz @StephVSherman
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 29th Episode 103: clinicalproblemsolving.com/morning-report…
W / Reshon Hadmon, Sonia Silinisky, & @AchantaAditya
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 29th Episode 103: clinicalproblemsolving.com/morning-report…
W / Reshon Hadmon, Sonia Silinisky, & @AchantaAditya

Let’s start with a problem representation:
A 30 y/o F presents w/ a 6-mon history of a nonproductive cough worse w/ activity, a recent-onset fever, blurred vision, dry eyes who was found to have uveitis, erythema nodosum, & crackles on PE along w/ hilar LAD & hypercalcemia
A 30 y/o F presents w/ a 6-mon history of a nonproductive cough worse w/ activity, a recent-onset fever, blurred vision, dry eyes who was found to have uveitis, erythema nodosum, & crackles on PE along w/ hilar LAD & hypercalcemia
Let's start with the cough.
A chronic cough in a 30 y/o? hmmm
Cough thinking about a pulmonary process (anywhere from nose to alveoli) but also thinking about GI and cardiac etiologies causing cough as well
A chronic cough in a 30 y/o? hmmm
Cough thinking about a pulmonary process (anywhere from nose to alveoli) but also thinking about GI and cardiac etiologies causing cough as well
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 27th Day 102: clinicalproblemsolving.com/morning-report…
w/ case presenter @sonyardavey and discussants Leticia Maciel & Andrew Sanchez
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 27th Day 102: clinicalproblemsolving.com/morning-report…
w/ case presenter @sonyardavey and discussants Leticia Maciel & Andrew Sanchez

Let’s start with a problem representation:
An 84-y/o M with a PMH of CAD with CABG, HTN, hypothyroidism, adeno carcinoma of the duodenum s/p Whipple and chemo currently in remission, & Carpal Tunnel Syndrome (CTS) p/w 10 days of scrotal/leg swelling and fatigue w/o CP or SOB
An 84-y/o M with a PMH of CAD with CABG, HTN, hypothyroidism, adeno carcinoma of the duodenum s/p Whipple and chemo currently in remission, & Carpal Tunnel Syndrome (CTS) p/w 10 days of scrotal/leg swelling and fatigue w/o CP or SOB
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 22nd Day 98: clinicalproblemsolving.com/morning-report…
w/ @sargsyanz @StephVSherman @TheRealDSrini AVi Sonnenschei & Sara Torres
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 22nd Day 98: clinicalproblemsolving.com/morning-report…
w/ @sargsyanz @StephVSherman @TheRealDSrini AVi Sonnenschei & Sara Torres

Let’s start with an initial problem representation:
A 31 yo M p/w 6 months of hematochezia, morning stiffness, diffuse symmetrical joint pains, & intermittent finger duskiness
A 31 yo M p/w 6 months of hematochezia, morning stiffness, diffuse symmetrical joint pains, & intermittent finger duskiness
intermittent duskiness? is this Raynaud's?
The overlap between GI and arthritis triggers spondyloarthopathies
BRBPR= lower GI bleed. Think colon masses/polyps, sigmoid diverticulosis (uncommon at this age but possible), anorectal disease (masses, hemorrhoids)
The overlap between GI and arthritis triggers spondyloarthopathies
BRBPR= lower GI bleed. Think colon masses/polyps, sigmoid diverticulosis (uncommon at this age but possible), anorectal disease (masses, hemorrhoids)
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
July 15th Day 93: clinicalproblemsolving.com/morning-report…
Chat recap of the #ClinicalPearls #VirtualMorningReport
Featuring: @sargsyanz @StephVSherman @tonlajr @AdamTapley
Teaching points overview by @sukritibanthiya
July 15th Day 93: clinicalproblemsolving.com/morning-report…
Chat recap of the #ClinicalPearls #VirtualMorningReport
Featuring: @sargsyanz @StephVSherman @tonlajr @AdamTapley
Teaching points overview by @sukritibanthiya

Before we start, if you didn't check out @_HarryPaul_ twitter thread from last wk, 👉👉
Now the initial PR:
A 60 y/o M w/ PMH of relapsing MS dx (last flare 4 yrs ago) p/w unsteadiness, trouble focusing & weightloss was tx for MS flare w/o improvement
Now the initial PR:
A 60 y/o M w/ PMH of relapsing MS dx (last flare 4 yrs ago) p/w unsteadiness, trouble focusing & weightloss was tx for MS flare w/o improvement
"difficulty focusing on objects" --> interesting
maybe he has diplopia, Check out this flow chart for this "blurry" topic
Is this JC virus reactivation with PML?natalizumab and some of the new oral agents can cause: iomcworld.org/open-access/na…
maybe he has diplopia, Check out this flow chart for this "blurry" topic
Is this JC virus reactivation with PML?natalizumab and some of the new oral agents can cause: iomcworld.org/open-access/na…

It's time for a slightly tardy #SpacedRepetition: @CPSolvers
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 10th Day 91: clinicalproblemsolving.com/morning-report…
w/ @AnnKumfer @DxRxEdu @rabihmgeha
Teaching points: @sukritibanthiya
Get ready for the @fernandbteich show
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 10th Day 91: clinicalproblemsolving.com/morning-report…
w/ @AnnKumfer @DxRxEdu @rabihmgeha
Teaching points: @sukritibanthiya
Get ready for the @fernandbteich show

But first, we want to acknowledge @_HarryPaul_ who gave us all something to reflect on. #MichaelHickson
washingtonpost.com/health/2020/07…
Thanks for stepping up and sharing Harry!
washingtonpost.com/health/2020/07…
Thanks for stepping up and sharing Harry!
Let’s start with a problem representation:
A 69-y/o F w/ a PMH of sinus cancer presents from an outside hospital with night sweats that started 4 wks ago along w/ rigors, fevers, nausea, early satiety, & weightloss found to have splenomegaly, lymphopenia, & elevated ESR/CRP
A 69-y/o F w/ a PMH of sinus cancer presents from an outside hospital with night sweats that started 4 wks ago along w/ rigors, fevers, nausea, early satiety, & weightloss found to have splenomegaly, lymphopenia, & elevated ESR/CRP
On day 14 of neutropenia, an astute ID fellow noted this finding (photo) while examining a patient with fever. Underlying AML and ongoing chemotherapy.
What do you suspect? What work up do you suggest? Details and #MayoIDQ MCQ to follow...
What do you suspect? What work up do you suggest? Details and #MayoIDQ MCQ to follow...

65M acute myeloid leukemia. Rx: CLAG-M. Prophy ACV, posaconazole, Levo, inhaled pentamidine
D14 neutropenia: fever / chills
Exam: onychomycosis, rapidly evolving lesions in arms and torso (photo)
You asked for skin biopsy. Blood culture will grow what fungus?
D14 neutropenia: fever / chills
Exam: onychomycosis, rapidly evolving lesions in arms and torso (photo)
You asked for skin biopsy. Blood culture will grow what fungus?
2/
Case diagnosis: disseminated fusariosis
Majority got the diagnosis correctly!
Blood culture: Fusarium sp.
Rx: AmBisome / voriconazole
Hope for neutrophil recovery!!!
Case diagnosis: disseminated fusariosis
Majority got the diagnosis correctly!
Blood culture: Fusarium sp.
Rx: AmBisome / voriconazole
Hope for neutrophil recovery!!!
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu, @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 2nd Day 86: clinicalproblemsolving.com/morning-report…
w/ @ABRezMed @hraza222 & Dr. Silinsky Krupnikov @Sharminzi @ArsalanMedEd
Case Overview by @AndreaAnampaG
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 2nd Day 86: clinicalproblemsolving.com/morning-report…
w/ @ABRezMed @hraza222 & Dr. Silinsky Krupnikov @Sharminzi @ArsalanMedEd
Case Overview by @AndreaAnampaG

Let’s start with a problem representation:
An 80 yo F presents with worsening fatigue x 1 month, 1 week of DOE, and “dizziness” was found to be anemic, hypercalcemic with an AKI, elevated Gamma Gap with a IgM monoclonal Spike, & increased serum viscosity
An 80 yo F presents with worsening fatigue x 1 month, 1 week of DOE, and “dizziness” was found to be anemic, hypercalcemic with an AKI, elevated Gamma Gap with a IgM monoclonal Spike, & increased serum viscosity
Time for some #SpacedRepetition: @CPSolvers
Chat recap of the #ClinicalPearls #VirtualMorningReport
June 29th Day 84: clinicalproblemsolving.com/morning-report…
w/ @RezidentMD @DxRxEdu @rabihmgeha
Case Overview by @haematognomist
Teaching points by @sukritibanthiya clinicalproblemsolving.com/wp-content/upl…
Chat recap of the #ClinicalPearls #VirtualMorningReport
June 29th Day 84: clinicalproblemsolving.com/morning-report…
w/ @RezidentMD @DxRxEdu @rabihmgeha
Case Overview by @haematognomist
Teaching points by @sukritibanthiya clinicalproblemsolving.com/wp-content/upl…
Let’s start with a problem representation:
A 30 yo M from Guatemala w/ a PMH of ETOH abuse who works in a warehouse presents w/ 1month of worsening SOB, non-productive cough, nausea, diarrhea, & 15 lb weight loss was found to be tachy, hypoxic, & tachypneic w/ 🔽 BS bilaterally
A 30 yo M from Guatemala w/ a PMH of ETOH abuse who works in a warehouse presents w/ 1month of worsening SOB, non-productive cough, nausea, diarrhea, & 15 lb weight loss was found to be tachy, hypoxic, & tachypneic w/ 🔽 BS bilaterally
thinking about dyspnea pyramid right off the bat - pulmonary (airway, vasculature, parenchyma, etc.), cardiac, “bad” blood (anemia, carboxyhemoglobinemia) and acid-base disorders
Lung>blood>Heart
Tachycardia always gets our attention as does the pulse ox
Lung>blood>Heart
Tachycardia always gets our attention as does the pulse ox
Time for some #SpacedRepetition: @CPSolvers
Chat recap of the #ClinicalPearls #VirtualMorningReport
June 26th Day 83: clinicalproblemsolving.com/morning-report…
w/ Neha Teekappanavar @DxRxEdu @rabihmgeha
Case Overview by @LindseyShipley8
Chat recap of the #ClinicalPearls #VirtualMorningReport
June 26th Day 83: clinicalproblemsolving.com/morning-report…
w/ Neha Teekappanavar @DxRxEdu @rabihmgeha
Case Overview by @LindseyShipley8
Let's start with an initial problem representation:
A 52 y/o F presents with 2 months of fatigue, 3 wks of mid back pain, foamy urine, hypersalivation, and swelling in her ankle and face
A 52 y/o F presents with 2 months of fatigue, 3 wks of mid back pain, foamy urine, hypersalivation, and swelling in her ankle and face
Enter ITAMED:
would look for systemic symptoms like weight loss, night sweats
Back pain age over 50 is a red flag to image
frothy urine...nephrotic?
foamy urine can indicate proteinuria although non-specific
clinical significance of foamy urine?ncbi.nlm.nih.gov/pmc/articles/P…
would look for systemic symptoms like weight loss, night sweats
Back pain age over 50 is a red flag to image
frothy urine...nephrotic?
foamy urine can indicate proteinuria although non-specific
clinical significance of foamy urine?ncbi.nlm.nih.gov/pmc/articles/P…
Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha @andressa__k @sargsyanz @StephVSherman @OpsBug @fernandbteich
Chat recap #ClinicalPearls #VirtualMorningReport
June 24th Day 80 clinicalproblemsolving.com/morning-report…
Case Overview @haematognomist
Chat recap #ClinicalPearls #VirtualMorningReport
June 24th Day 80 clinicalproblemsolving.com/morning-report…
Case Overview @haematognomist
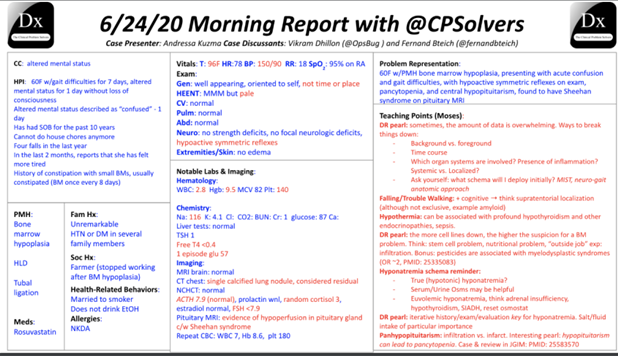
Let's start with a Problem Representation:
A 6o y/o F presents with 10 yrs of SOB, recent falls the last few months, increasing fatigue, constipation (1 BM every 8 days), and new-onset AMS found to have pancytopenia, 🔽Na, 🔽Glu, 🔽 Free T4, 🔽cortisol
A 6o y/o F presents with 10 yrs of SOB, recent falls the last few months, increasing fatigue, constipation (1 BM every 8 days), and new-onset AMS found to have pancytopenia, 🔽Na, 🔽Glu, 🔽 Free T4, 🔽cortisol
From the get-go: Gait difficulties for 7 days, AMS, constipation
Enter MIST pneumonic for AMS
Hypercalcemia links constipation and AMS but Hyper CA doesn't explan dyspnea
she will have polyuria w/her hypercalcemia
ncbi.nlm.nih.gov/books/NBK27912…
Enter MIST pneumonic for AMS
Hypercalcemia links constipation and AMS but Hyper CA doesn't explan dyspnea
she will have polyuria w/her hypercalcemia
ncbi.nlm.nih.gov/books/NBK27912…
Time for some #SpacedRepetition: @CPSolvers
Chat recap of the #ClinicalPearls #VirtualMorningReport
w/ @StephVSherman @DxRxEdu @rabihmgeha
June 22th Day 79: clinicalproblemsolving.com/morning-report…
Case Overview by @haematognomist
Chat recap of the #ClinicalPearls #VirtualMorningReport
w/ @StephVSherman @DxRxEdu @rabihmgeha
June 22th Day 79: clinicalproblemsolving.com/morning-report…
Case Overview by @haematognomist

Prior to case @medrants shared some pearls on the prior VMR case:
Patients with Lemierre syndrome have a high risk of new thromboembolic complications, clinical sequelae and death: an analysis of 712 cases onlinelibrary.wiley.com/doi/full/10.11…
Patients with Lemierre syndrome have a high risk of new thromboembolic complications, clinical sequelae and death: an analysis of 712 cases onlinelibrary.wiley.com/doi/full/10.11…
Let's start with an initial problem representation:
A 49-yo M was found unresponsive laying in a park w/ an almost empty trazodone bottle that was filled layer, he was obtunded on exam w/o signs of trauma and found to have ⏫AG, ⏫Cr, ⏫ Osm Gap, ⏫QTc
A 49-yo M was found unresponsive laying in a park w/ an almost empty trazodone bottle that was filled layer, he was obtunded on exam w/o signs of trauma and found to have ⏫AG, ⏫Cr, ⏫ Osm Gap, ⏫QTc