Discover and read the best of Twitter Threads about #eol
Most recents (13)
#EoL care staff need to talk about restlessness prior to death, including it in preparation. Although it's not common, it's highly distressing if companions don't understand it.
Here's an edit of my recent public info post on Facebook, where I don't use medical language.
1/
Here's an edit of my recent public info post on Facebook, where I don't use medical language.
1/

'Terminal agitation' isn't a diagnosis, but it describes muddled thinking with unusual behaviours that occasionally happens in a person close to death.
Understanding what might be happening helps us to respond calmly. *
2/



Understanding what might be happening helps us to respond calmly. *
2/




1. Towards death, the brain is losing consciousness. Most people are deeply unconscious & peaceful, but a few spend time more alert (again, usually peaceful). Some of these intermittently experience a kind of neither-awake-nor-asleep state.
3/
3/
Thread about end of life decisions: #EOL
A couple weeks ago, I had a good friend diagnosed with an aggressive glioblastoma (brain tumor). She underwent surgery. Of course they couldn't get it all and I visited to help her and her children decide on the next steps. 1/x
A couple weeks ago, I had a good friend diagnosed with an aggressive glioblastoma (brain tumor). She underwent surgery. Of course they couldn't get it all and I visited to help her and her children decide on the next steps. 1/x
At her follow up, we didn’t know the official diagnosis. Based on the odds I did all the research on glioblastoma treatments. I figured once we had the full picture, we could decide the next steps. Despite surgery, her brain worked well and she had an excellent attitude. 2/x
The neurosurgeon came in first. He informed us it was a glioblastoma (glad I went with the odds). He said she needed the standard six weeks radiation treatment and chemotherapy, and that they were going to fit her with an “Optune” device (very cumbersome equipment.) 3/x
Here are some lessons learned from our past engagements; see it as an easy checklist on what not to do. #LessonsLearned ✅
1) MFA (Multi-Factor-Authentication) being not fully implemented or non-existent at all
While some attackers steal MFA tokens, it is rare! 📱 #MFA
While some attackers steal MFA tokens, it is rare! 📱 #MFA
Our new paper is out !
We explore which aspects influence health professionals´ decisions regarding EoL decisions and care for cancer patients in Colombia. #palliativecare @palliativewise @BMC_series #cancercare #patientcare
doi.org/10.1186/s12904…
Starting thread ... 🧵
We explore which aspects influence health professionals´ decisions regarding EoL decisions and care for cancer patients in Colombia. #palliativecare @palliativewise @BMC_series #cancercare #patientcare
doi.org/10.1186/s12904…
Starting thread ... 🧵
We did a qualitative descriptive-exploratory study based on phenomenology using semi-structured interviews incluiding several professionals´ and several urban hospitals. Main results 👇
Professionals consider :
Professionals consider :
👉Patient's clinical condition, cultural and social context, in particular treating indigenous patients requires special skills, so training in discussing EoL is extremely important.
👉Many patients deny their imminent death which hampers shared open conversations.
👉Many patients deny their imminent death which hampers shared open conversations.
I'm so saddened by a story shared with me today.
Just this week, a paramedic was called to administer CPR to a 100yr old woman, as requested by the RN in the aged care home, on the family's instructions. There was no advance care plan in place. (1/7)
Just this week, a paramedic was called to administer CPR to a 100yr old woman, as requested by the RN in the aged care home, on the family's instructions. There was no advance care plan in place. (1/7)
Fortunately, the paramedic that attended the aged care home was a courageous young woman who managed to get the resident's family on the phone, explain the trauma that CPR would cause, and with their consent, the lady was allowed to die in peace. (2/7)
There are so many things deeply wrong with this scenario.
First - the family. Unaware that this woman was in the last stages of her life. Unsupported & unprepared for the decisions they needed to make on her behalf.
Family dynamics = key drivers of non-beneficial treatment (3/7)
First - the family. Unaware that this woman was in the last stages of her life. Unsupported & unprepared for the decisions they needed to make on her behalf.
Family dynamics = key drivers of non-beneficial treatment (3/7)
El otro día hablaba de uno de mis temas regalones, el Fin de la Vida en los servicios de Urgencia, con los residentes de #MedEmergGuatemala 🇬🇹
En estos tiempos pandémicos, parece más relevante que nunca...
En estos tiempos pandémicos, parece más relevante que nunca...

A sugerencia d @interneurona unas perlitas sobre el #FinDeLaVida #EOL en los Servicios de Urgencia en este hilo🧵.
Disclaimer: no soy d esas personas q creen q tienen la verdad universal, sino lo contrario. Estos son *mis pensamientos* sobre el tema, bienvenidos los aportes!
1/x
Disclaimer: no soy d esas personas q creen q tienen la verdad universal, sino lo contrario. Estos son *mis pensamientos* sobre el tema, bienvenidos los aportes!
1/x
Urgenciólogos estamos formados para enfrentar/tratar emergencias+muertes *espectaculares*.
Politrauma, Shock, Sepsis, IAM, ACV, Intox...
PERO muchos d nuestros pacientes van a morir de muertes *subtaculares* s/ sangre, gritos, ni desastre.
Y no estamos preparados para eso 😳
2/x
Politrauma, Shock, Sepsis, IAM, ACV, Intox...
PERO muchos d nuestros pacientes van a morir de muertes *subtaculares* s/ sangre, gritos, ni desastre.
Y no estamos preparados para eso 😳
2/x
@DukePallCare SUCCESS! Journal Club Time Machine: Speed Dating with the Classics. Format - everyone in attendance (MS2-Attending) teaches a classic article for 4 minutes, it is put in context by someone old for 1-2 min, and we move on. Here's the list! A #HPC thread:
No 1 - SUPPORT Trial: pubmed.ncbi.nlm.nih.gov/7474243/. 5 AMCs. Docs don't know pt's CPR preference, many DNRs within 2d of death, lots of ICU time and pain. RN led intervention gives docs data. Centers around communication. NO CHANGE IN KEY METRICS.
No 2 - Prognostication: pubmed.ncbi.nlm.nih.gov/10678857/. Docs of pts referred to #hospice asked for assessment of prognosis. Only 20% accurate (+/- 33%) with most over-optimistic. Average miss factor of 5.3! Longer pt/doc relationship = worse prognostication accuracy (#LoveThemTooMuch)
1/ End of Life (#EOL) Pro-Tip: flipping it. 👍
Sick patient asks, “Doc, how long am I gonna live?”
It’s an impossible ? to answer, but (a) don’t miss opportunity to help her & (b) don’t get backed into corner. I was taught by Joanne Lynn to flip the question!
#MedTwitter
Sick patient asks, “Doc, how long am I gonna live?”
It’s an impossible ? to answer, but (a) don’t miss opportunity to help her & (b) don’t get backed into corner. I was taught by Joanne Lynn to flip the question!
#MedTwitter

2/ End of Life (#EOL)
The FLIP: After adequate verbal prep, “So Mrs. Smith, I can’t tell you how long you will live, but I can help you understand how quickly you might die.” Hours to days, days to weeks...
This helps her realize every day is a gift day & plan.
#pulmcc #MedEd
The FLIP: After adequate verbal prep, “So Mrs. Smith, I can’t tell you how long you will live, but I can help you understand how quickly you might die.” Hours to days, days to weeks...
This helps her realize every day is a gift day & plan.
#pulmcc #MedEd

3/fin End of Life (#EOL)
Intern asked: “How do you know when to invoke this FLIP?”
My method: “I imagine I’m walking in for rounds & you tell me Mrs. Smith died last night & I realize I’m not surprised. Then I try to make sure she knows...
It’s a morph of the surprise question.
Intern asked: “How do you know when to invoke this FLIP?”
My method: “I imagine I’m walking in for rounds & you tell me Mrs. Smith died last night & I realize I’m not surprised. Then I try to make sure she knows...
It’s a morph of the surprise question.

I'm thinking about the chatter about #COVIDー19 #EOL conversations. There's a risk here that we should say out loud. The moral satisfaction that can come to clinicians from encouraging a "good" death may mix the role of the Crisis Triage Officers (making fair and just
assessments for a community of how to share limited life support capacity) with the clinician (seeking care that is helpful and true to their specific patient as a person. For an individual patient, COVID is just ARDS. It is not the moral distress and even discomfiture (used
with its dictionary definition) that we experience about this awful pandemic. It is ARDS. So if walking the path of treatment for ARDS is true to them as a person, the bedside clinician should offer it unless and until a formal Triage team is forced to restrict such care.
Here's a cry from the heart. #eol Twitter, this is so real: @chippety knows this is the dying time & can't deal with books, articles, long diatribes. This is about getting to the heart of supporting our loved ones at the end of life.
Practical things:
Where will he be cared for? How can companions ensure he has company when he wishes, time to rest, help to move around? Support for his dearest people? Help with laundry, shopping, meals?
Make a list of jobs.
Write rotas.
People want to help but don't know how.
Where will he be cared for? How can companions ensure he has company when he wishes, time to rest, help to move around? Support for his dearest people? Help with laundry, shopping, meals?
Make a list of jobs.
Write rotas.
People want to help but don't know how.
Plan ahead things:
Does he have a named person as his Health Attorney in case he can't speak for himself some days?
Takes a few days to get all the signatures & register the form: gov.uk/government/pub…
Does he have a named person as his Health Attorney in case he can't speak for himself some days?
Takes a few days to get all the signatures & register the form: gov.uk/government/pub…
Some time ago, I saw a pt with severe untreated suffering at #EOL alongside aggressive & unproven life-prolonging interventions. When I asked the medical team, they said they were doing “what the family wanted.”
Sharing some of my thoughts about this below 👇🏾👇🏾👇🏾
Sharing some of my thoughts about this below 👇🏾👇🏾👇🏾
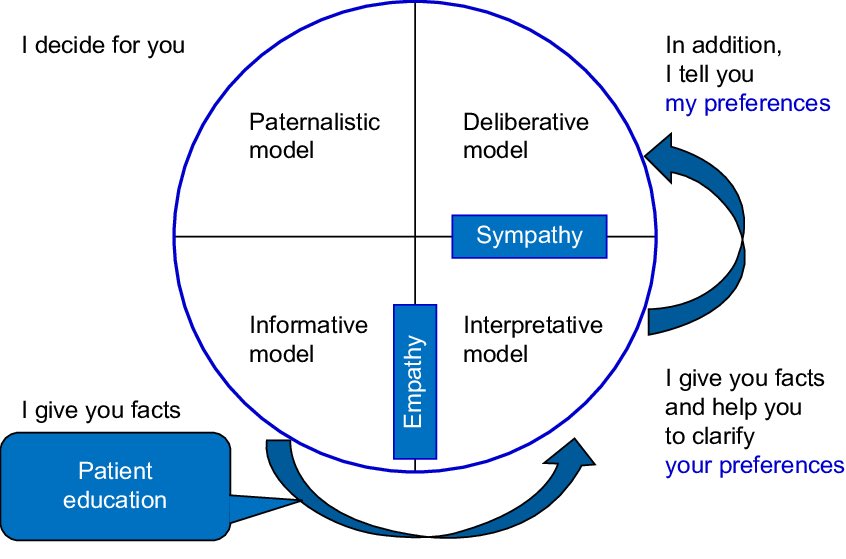
1/ Rejecting paternalism does not imply that we take ourselves out of the decision making process altogether. We should always work together with our pts & families rather than just “doing what they want.”
#hpm #hapc #bioethics
#hpm #hapc #bioethics
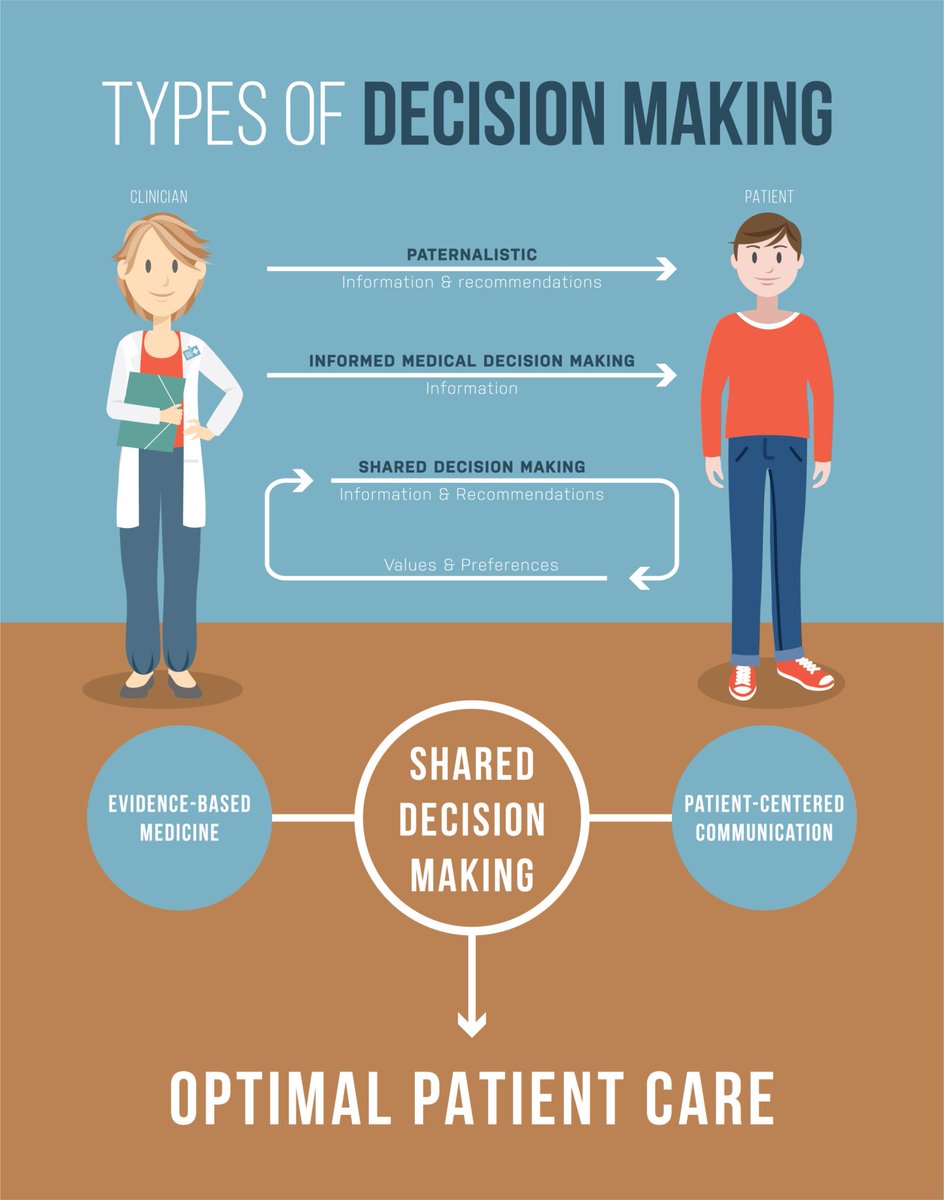
2/ We should move towards a “deliberative” rather than an “informative” model of decision making. Pts should share values/expectations & we propose medical treatments. It is crucial for all HCPs to have better training on having #goalsofcare conversations.
#hpm #hapc #bioethics
#hpm #hapc #bioethics
#TipsForNewDocs
Some patients are sick enough to die. They may pull through. They might not.
Say 'sick enough to die' to pt & family. Not 'serious.' Not 'critical.' Not 'unstable.' Name death as a possibility, & plan good #eol care in parallel with current treatment plan.
1/
Some patients are sick enough to die. They may pull through. They might not.
Say 'sick enough to die' to pt & family. Not 'serious.' Not 'critical.' Not 'unstable.' Name death as a possibility, & plan good #eol care in parallel with current treatment plan.
1/
If your patient is sick enough to die, get support from your seniors &/or pall care team.
Patients who see the pall care team are not obliged to die.
Pall care can help you with parallel planning, support pt/family/staff (you!), in ER, wards or ICU.
2/
Patients who see the pall care team are not obliged to die.
Pall care can help you with parallel planning, support pt/family/staff (you!), in ER, wards or ICU.
2/
A common complaint from families when patient dies is 'we didn't realise s/he might die!'
They are told about sepsis/low oxygen sats/hypotension/poor blood supply to vital organ(s) but this doesn't communicate 'sick enough to die.'
Use your D-words.
3/
They are told about sepsis/low oxygen sats/hypotension/poor blood supply to vital organ(s) but this doesn't communicate 'sick enough to die.'
Use your D-words.
3/
The other night at the hospital, I witnessed some shocking behavior & sub par care by a night shift #hospice #nurse-Hospice nurses ensure a dying patient receives dignified #EOL while being kept as comfortable as possible. For 12 hours -2/28-3/1, Melissa didn't get either. THREAD
I was sitting with Melissa, trying to calm her, she was agitated. RN Deb came in. She looked at me & asked who I was. Due to her tone, I told her I was family. She wanted to know who was staying over. We were curtly told only 2 were allowed, not 4. SHE was mistaken. #Hospice
Michele, patients mother very upset. RN Deb yelled at Melissa's Nieces. Told the little girls they were very bad & didn't belong up here. The girls weren't misbehaving. They weren't doing anything wrong, nor unattended in the common area of the #PalliativeCare #Hospice wing
