Discover and read the best of Twitter Threads about #hemepath
Most recents (24)
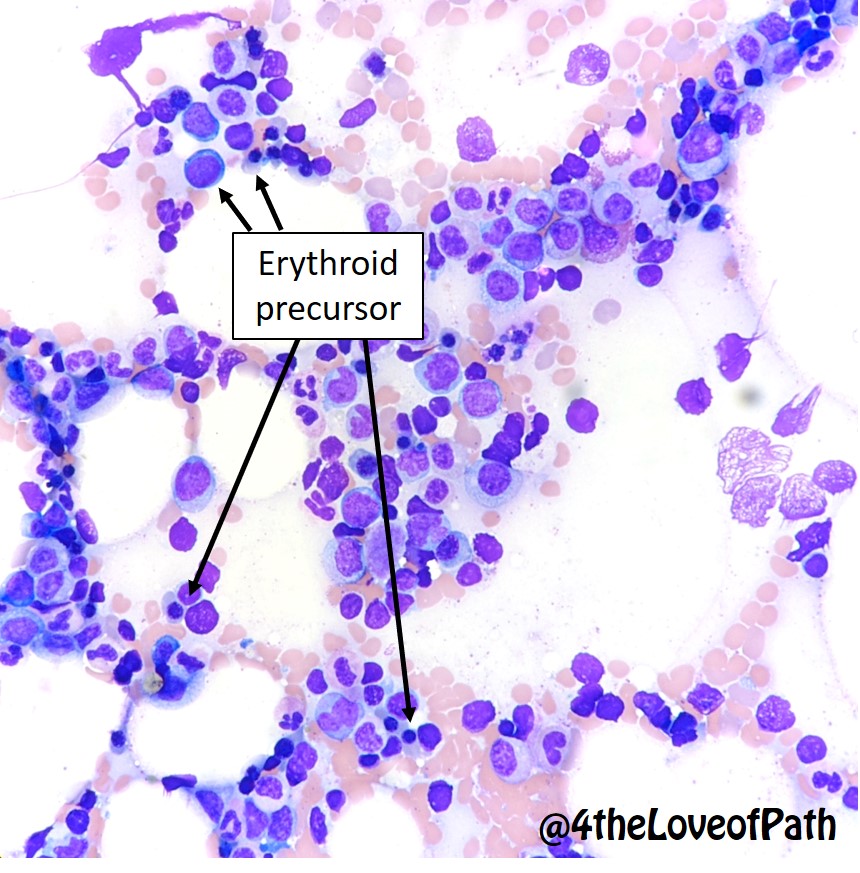
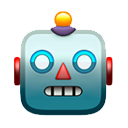
A #hemepath case to show why a myeloid FISH panel alone is not sufficient for AML Dx/prognosis
This monocytic AML had no evidence of del(7q) on FISH but had del(7)(q32) in 19/20 metaphases on karyotype
But Why?? #leusm 1/3


This monocytic AML had no evidence of del(7q) on FISH but had del(7)(q32) in 19/20 metaphases on karyotype
But Why?? #leusm 1/3

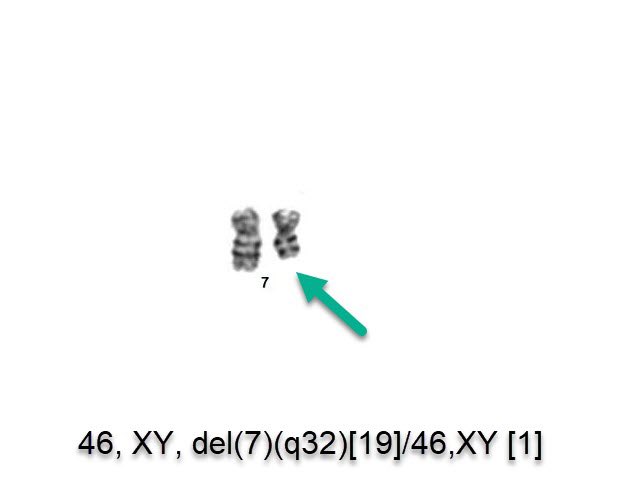
Because the @AbbottNews VYSIS D7S486/ CEP7 FISH PROBE KIT used in our FISH probes hybridize to centromere of ch. 7 (to detect monosomy 7)
& 7q31 region of the long arm of ch.7… so it does not detect a deletion telomeric to 7q31 (in this case 7q32)… why do we care? #hemepath 2/3
& 7q31 region of the long arm of ch.7… so it does not detect a deletion telomeric to 7q31 (in this case 7q32)… why do we care? #hemepath 2/3

Interestingly, ELN 2022 only considers monosomy 7 (not del7q) as adverse-risk.. bit.ly/3h2QGwQ
But this is debatable as they also recommend classifying del7q as myelodysplasia-related and many studies show del7q is ass/w poor prognosis 3/3 #hemepath

But this is debatable as they also recommend classifying del7q as myelodysplasia-related and many studies show del7q is ass/w poor prognosis 3/3 #hemepath


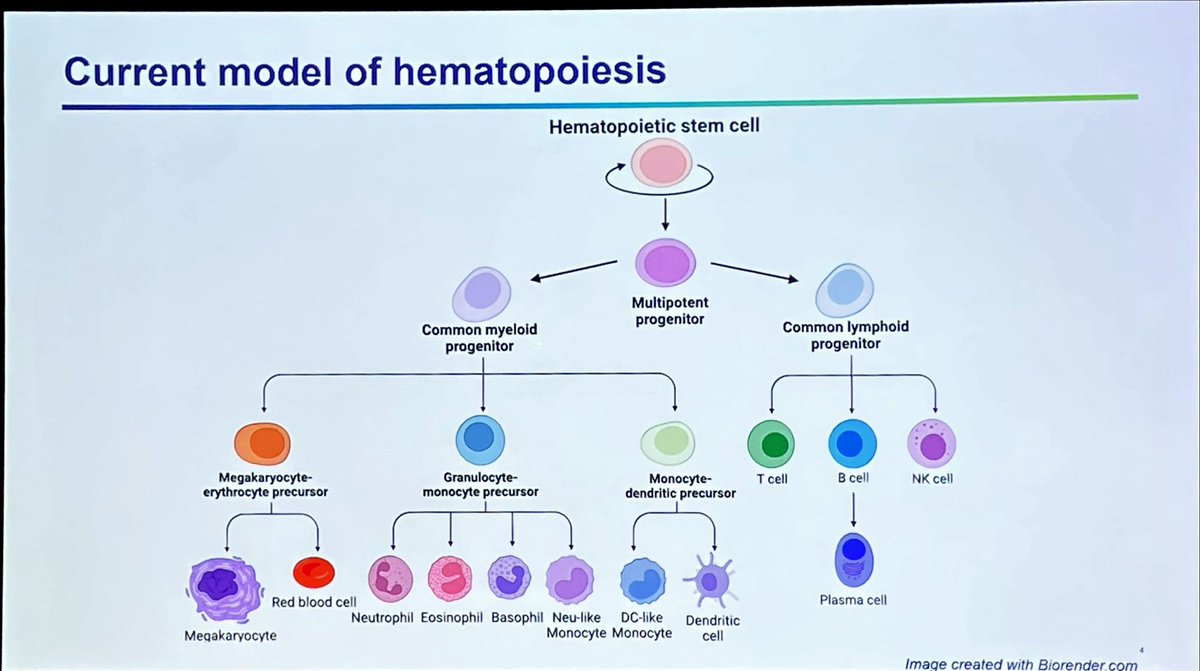
Best way to recognize pathological/neoplastic immunophenotypic changes is having a good grip on immunophynotypic variations in reactive/regenerative conditions… summarizing #FlowICCS22 plenary session 3 here👇🏻 🧵1/ #hemepath 

Normal granulocytic maturation patterns…. Plots follow maturation from promyelocyte (*) to neutrophils #flowiccs22 #hemepath 2/ 



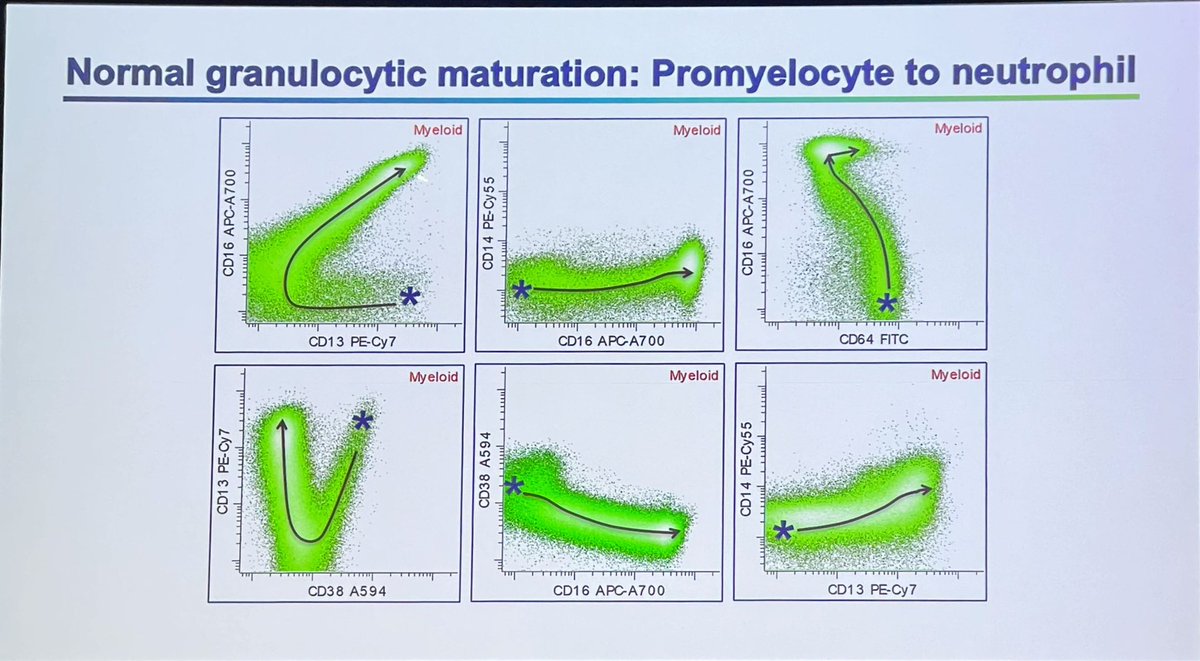
Here are phenotypic changes post GCSF therapy compared to Normal…. Don’t over-interpret this pattern as abnormal myeloid maturation #flowiccs22 #hemepath 3/ promyelocyte (*) to neutrophil 

@AaronGoodman33 Typical cytomorphology is characterized by “blasts” with hand mirror (red arrow, cytoplasm to the side) or pearl necklace (green arrow, small cytoplasmic vacuoles around nucleus) appearance #bpdcn #hemepath #RareDisease #WHOHEME 1/ 



@AaronGoodman33 Skin and lymph node are most common extramedullary sites of involvement. Skin infiltrate is usually dermal with an appreciable “grenz zone” (uninvolved band b/w dermis and epidermis).. Lymph node typically has diffuse or paracortical involvement #hemepath #WHOHEME #BPDCN 



@AaronGoodman33 Bone marrow involvement can be interstitial, nodular and leukemic or a-leukemic. This was an example of a leukemic case @JoeKhouryMD and I published in @BloodJournal #bloodwork bit.ly/3JUBls7 @ASH_hematology #imagebank #WHOHEME #hemepath #bpdcn 3/ 

One of the difficult aspects of #hemepath training is time management in a high-paced/demanding environment & the ability to multitask effectively while learning a difficult discipline. Every yr I offer our fellows helpful tips I’ve learned so far 🧵👇🏻More tips welcome,pls add 1/ 

Get rid of paper…
Don’t do anything twice
Take ownership of your cases… they are just as much yours as they are your faculty’s
Don’t do anything twice
Take ownership of your cases… they are just as much yours as they are your faculty’s

Use online learning tools… like great #hemepath modules here on @PathElective @KMirza @cullen_lilley 

Just another ordinary day at #hemepathMDA … 🤯
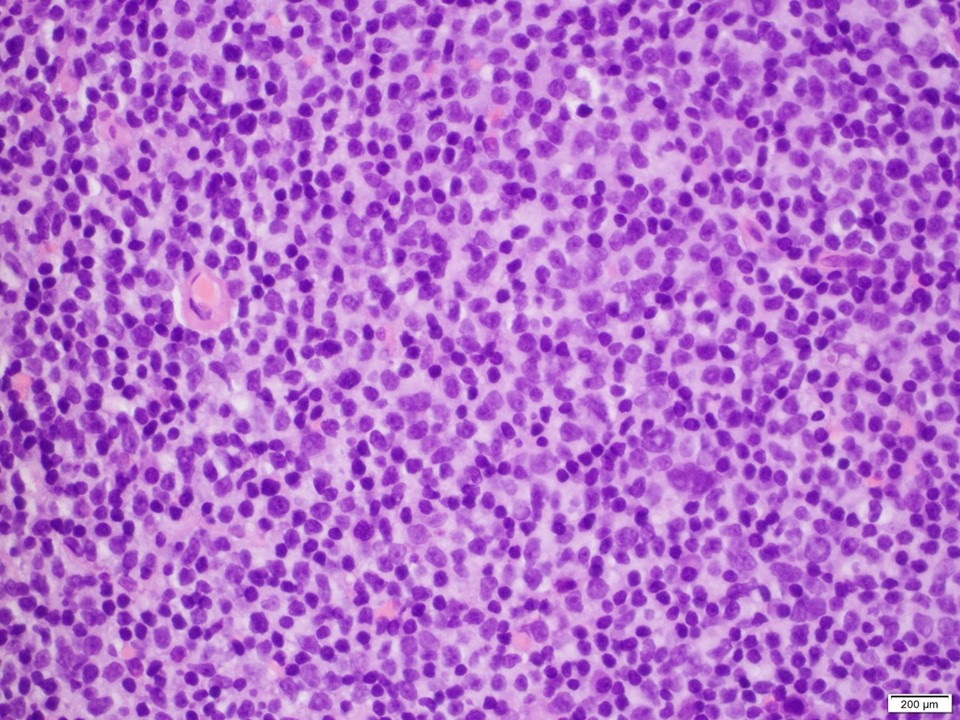
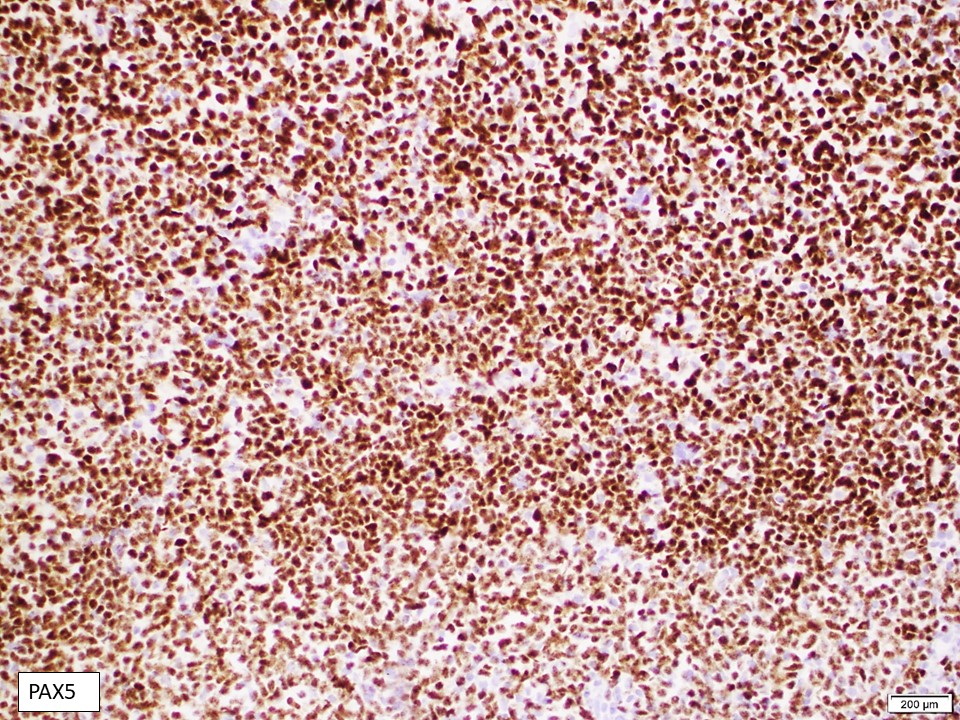
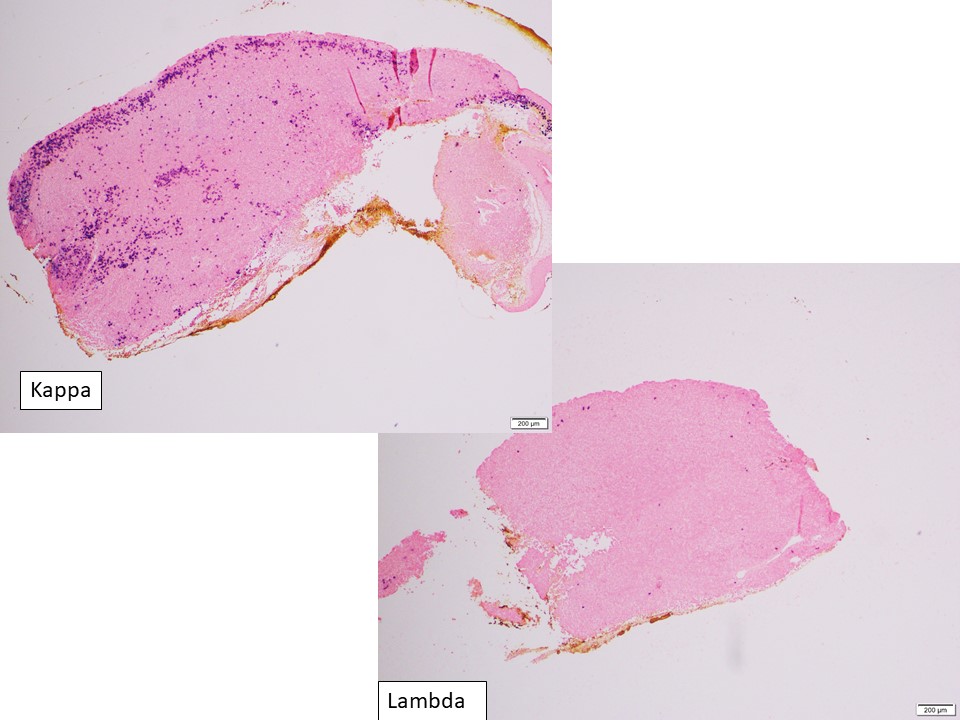
60-70 y/o woman
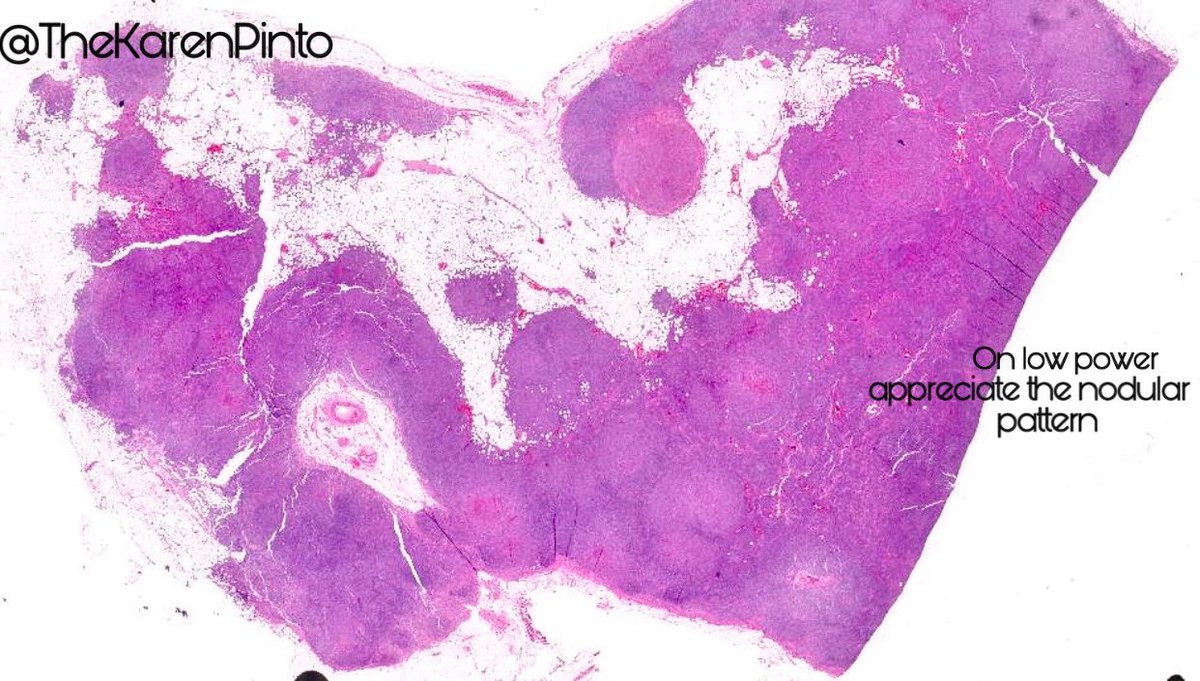
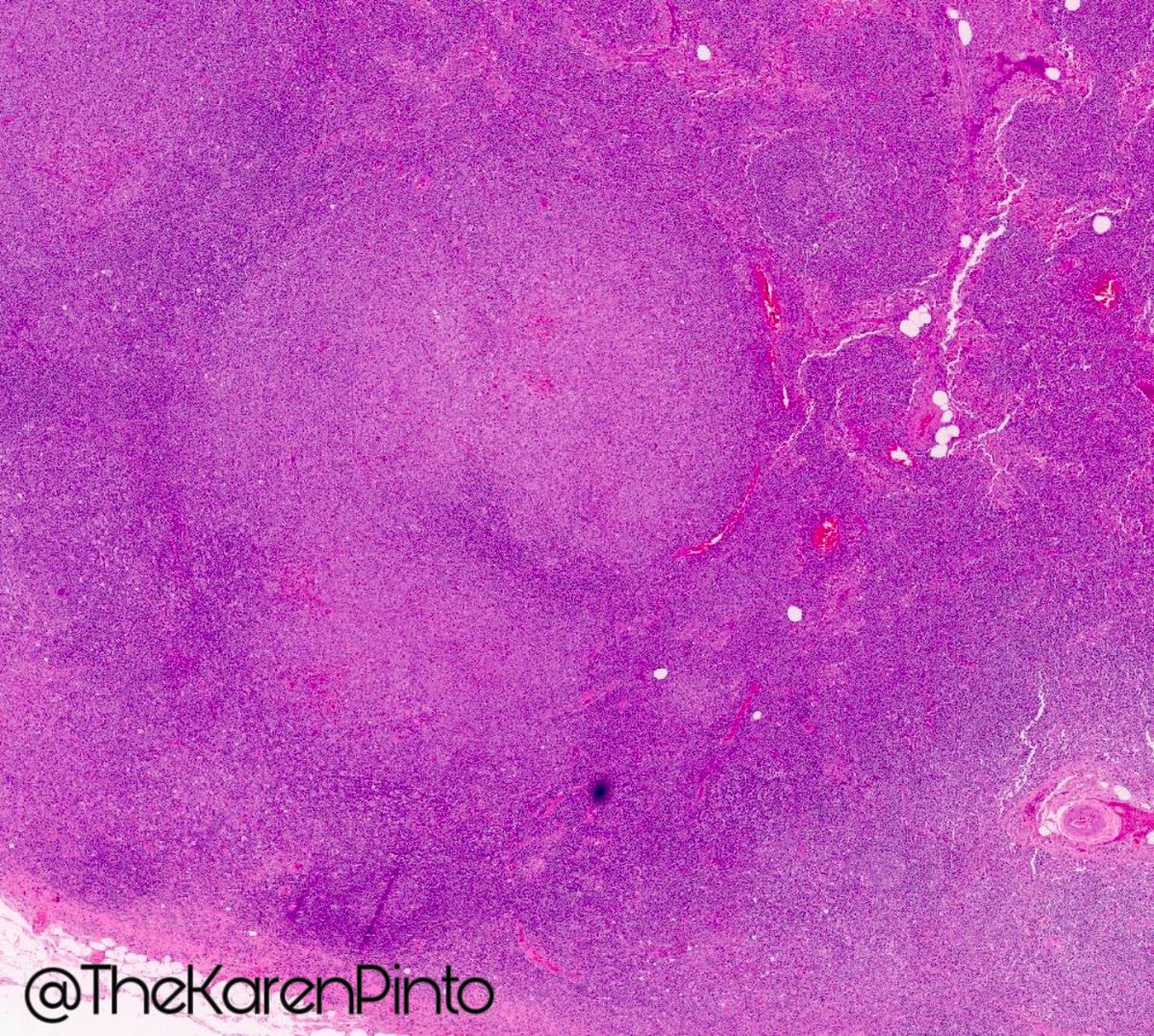
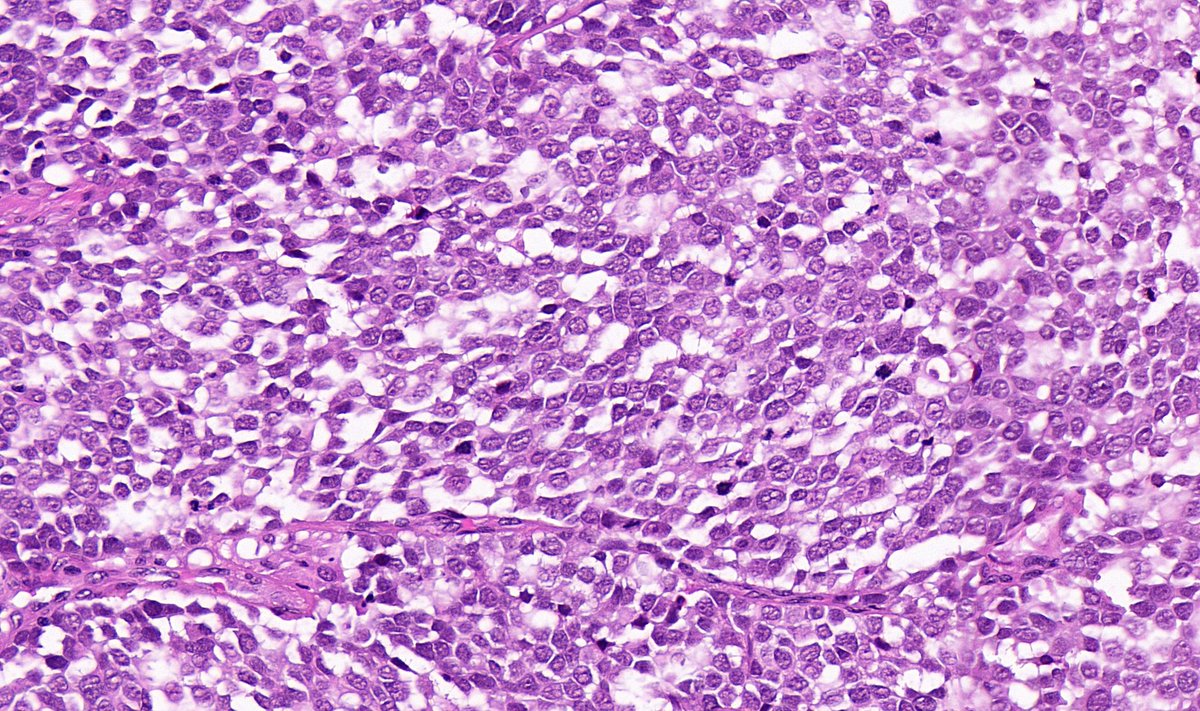
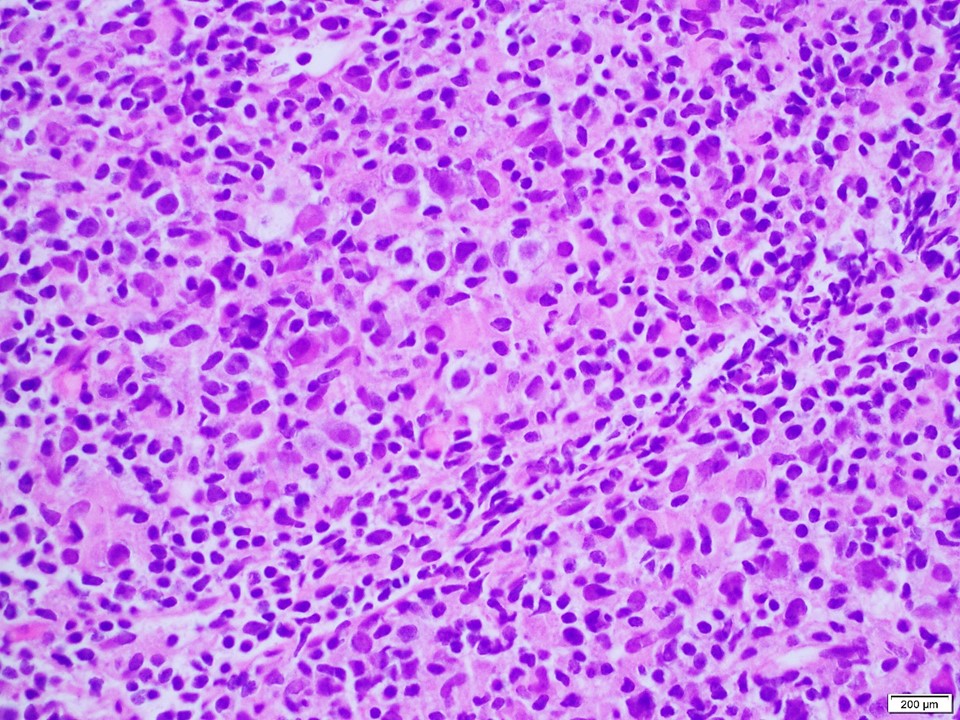
To all brave #hemepath aficionados how would you classify this case?
Poll and individual high quality images below. Pls comment if you’re feeling particularly brave today, let’s talk new #WHO 😎



60-70 y/o woman
To all brave #hemepath aficionados how would you classify this case?
Poll and individual high quality images below. Pls comment if you’re feeling particularly brave today, let’s talk new #WHO 😎



What’s your dx?
If you follow me, you know I love tweeting about #HemePath and lately #AML subtypes🩸
So far, I’ve covered the subtypes of AML with recurrent genetic abnormalities (per WHO 2016) - see below if you’re interested! ⬇️
Looking forward to more HemePath #tweetorials in the future!
So far, I’ve covered the subtypes of AML with recurrent genetic abnormalities (per WHO 2016) - see below if you’re interested! ⬇️
Looking forward to more HemePath #tweetorials in the future!

AML with mutated NPM1
AML with t(8;21)(q22;q22.1) RUNX1::RUNX1T1
🩸#HemePath AML subtype #PathTweetorial 🧵
Which cytogenetic/molecular finding is most consistent with this morphology? (Poll⬇️)
#PathTwitter #MolecularPath #MedEd @MayoClinicPath
(P.S. Always learning - I welcome any feedback!)

Which cytogenetic/molecular finding is most consistent with this morphology? (Poll⬇️)
#PathTwitter #MolecularPath #MedEd @MayoClinicPath
(P.S. Always learning - I welcome any feedback!)

Which cytogenetic/molecular finding is most consistent with this morphology? AML with…
The many faces of plasma cell neoplasm, diagnostic challenges of the great imitator in #hemepath ➡️bit.ly/3B3jMC1 with @ljmedeirosMD & @ShiminHuMDPhD #mmsm #lymsm #pathtwitter #leusm 

1) The small cell variant (mimicking B-cell lymphoma, particularly mantle cell lymphoma➡️CyclinD1 positive) #hemepath #pathtwitter 

The story of 1 day in the life of a #hematopathologist… I’m too exhausted to make a fancy educational thread but here are some amazing 🔬 pics for your viewing pleasure. I diagnosed all cases in one day 🤯 only at @MDAndersonNews Happy almost weekend people 🥂 #hemepath 🧵 1/n 

Myeloproliferative neoplasm w/ concurrent BCR::ABL1 and JAK2 V617F ..the megekaryocyte morphology is clue to something beyond CML #mpnsm #PathOutPic 2/ 





BPDCN with perfect so-called “hand mirror” (red) and “pearl necklace” (black) morphology #BPDCN #PathOutPic 3/ 

Happy to share our latest paper w/ @SibaElHussein as lead author, out today in @BMTjournal ⚡️Acquired WT1 mutations contribute to relapse of NPM1mut AML following allogeneic hematopoietic stem cell transplant rdcu.be/cEuxv #hemepath #leukemia #hemepathMDA 

WT1 mutations are present in ~7% of de novo AML, are typically Lof mutation involving exons 7-9 of the gene. They frequently (~15%) co-occur w/ NPM1mut & have detrimental impact in this setting, shown by @AkEisfeld and colleagues in bit.ly/3eWQtXw @LeukemiaJnl 

We studies a cohort of de novo NPM1-mut AML. 7% had concurrent WT1 mutations at baseline. 22% (15/67) relapsed; 4 (27%) with newly acquired Lof WT1-mut. Illustrated by @furudateken 

Based on the initial images only, what is your first impression?
(1/6) Future #dermpath star, @DermpatGal, & I have put together an illustration of hematologic findings in "Drug Reaction with Eosinophilia & Systemic Symptoms" (DRESS) @AjHematology ➡️ bit.ly/3u9WvLa
#hemepath #pathtwitter @Pathology_URMC 🔬
#Tweetorial ⬇️
#hemepath #pathtwitter @Pathology_URMC 🔬
#Tweetorial ⬇️

(2/6) Drug metabolites (commonly of anti-anticonvulsant medication) are thought to stimulate T-cells leading to a florid immune response/ or cause viral activation (HHV6) leading to downstream immune activation
(Pathogenesis of DRESS➡️bit.ly/3F3uKJp @MDPIOpenAccess )
(Pathogenesis of DRESS➡️bit.ly/3F3uKJp @MDPIOpenAccess )

#Pathologists ♥️ eosinophils.
We love scanning for them in a skin rash, admiring them when they infiltrate a tumor, & even counting them in esophageal biopsy. 🔬
But what do you know about eosinophils in the blood? 🤔
1/
#pathbracket #hemepath #pathtweetorial @EmoryPathology
We love scanning for them in a skin rash, admiring them when they infiltrate a tumor, & even counting them in esophageal biopsy. 🔬
But what do you know about eosinophils in the blood? 🤔
1/
#pathbracket #hemepath #pathtweetorial @EmoryPathology

If the answer is "not much 🤷🏼♀️", then you're in luck, because the subject of my 2nd #pathtweetorial is:
🥁🥁🥁
🩸 Approach to Peripheral Blood Eosinophilia 🩸
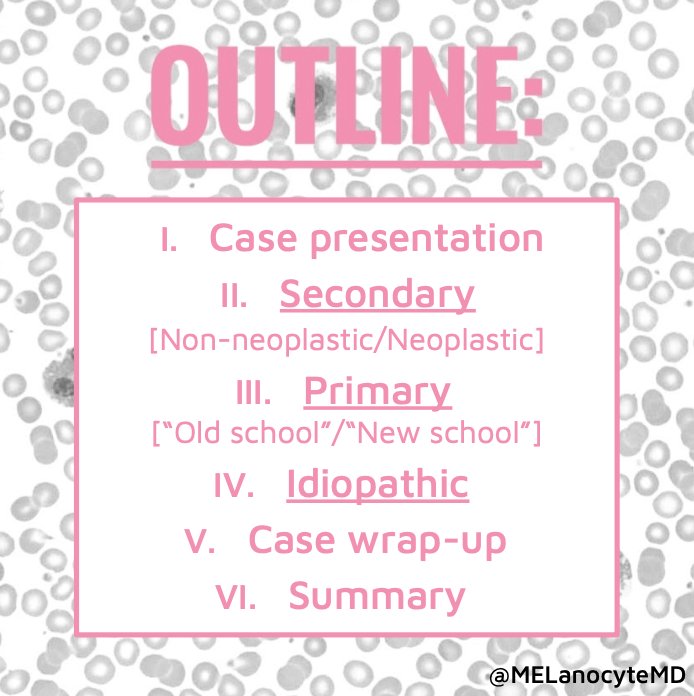
Here's a brief outline of what I'll be discussing:
2/
🥁🥁🥁
🩸 Approach to Peripheral Blood Eosinophilia 🩸
Here's a brief outline of what I'll be discussing:
2/
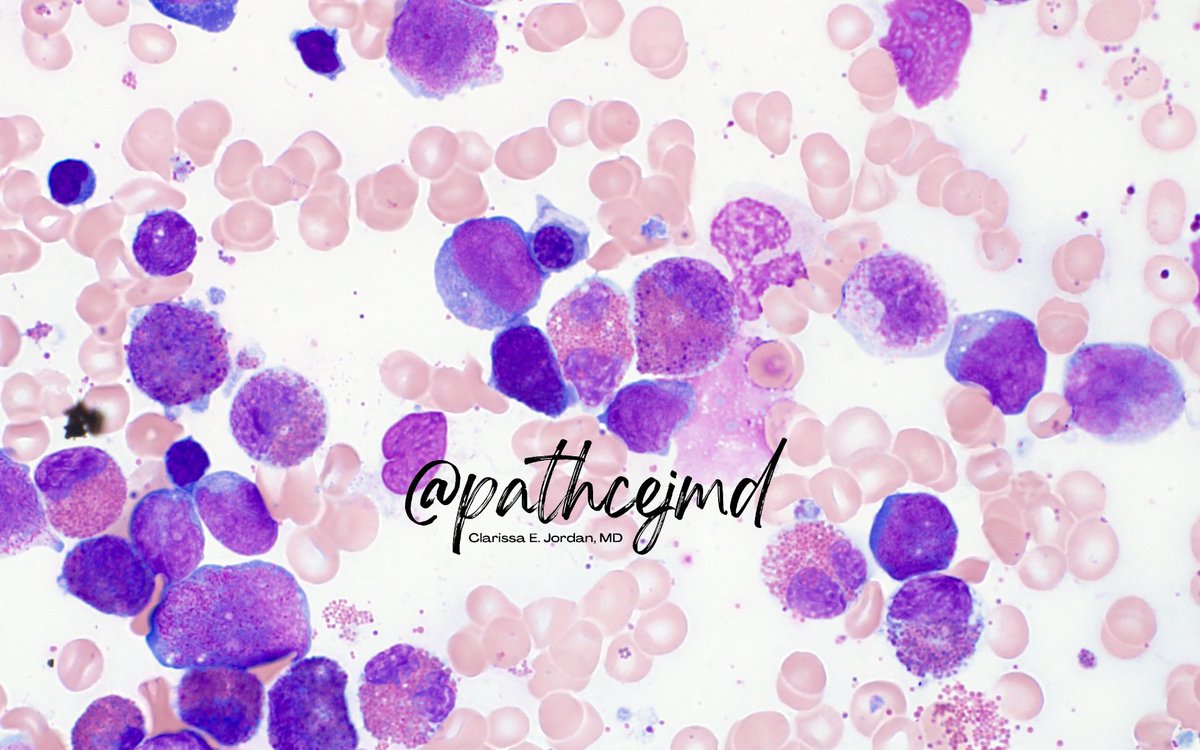
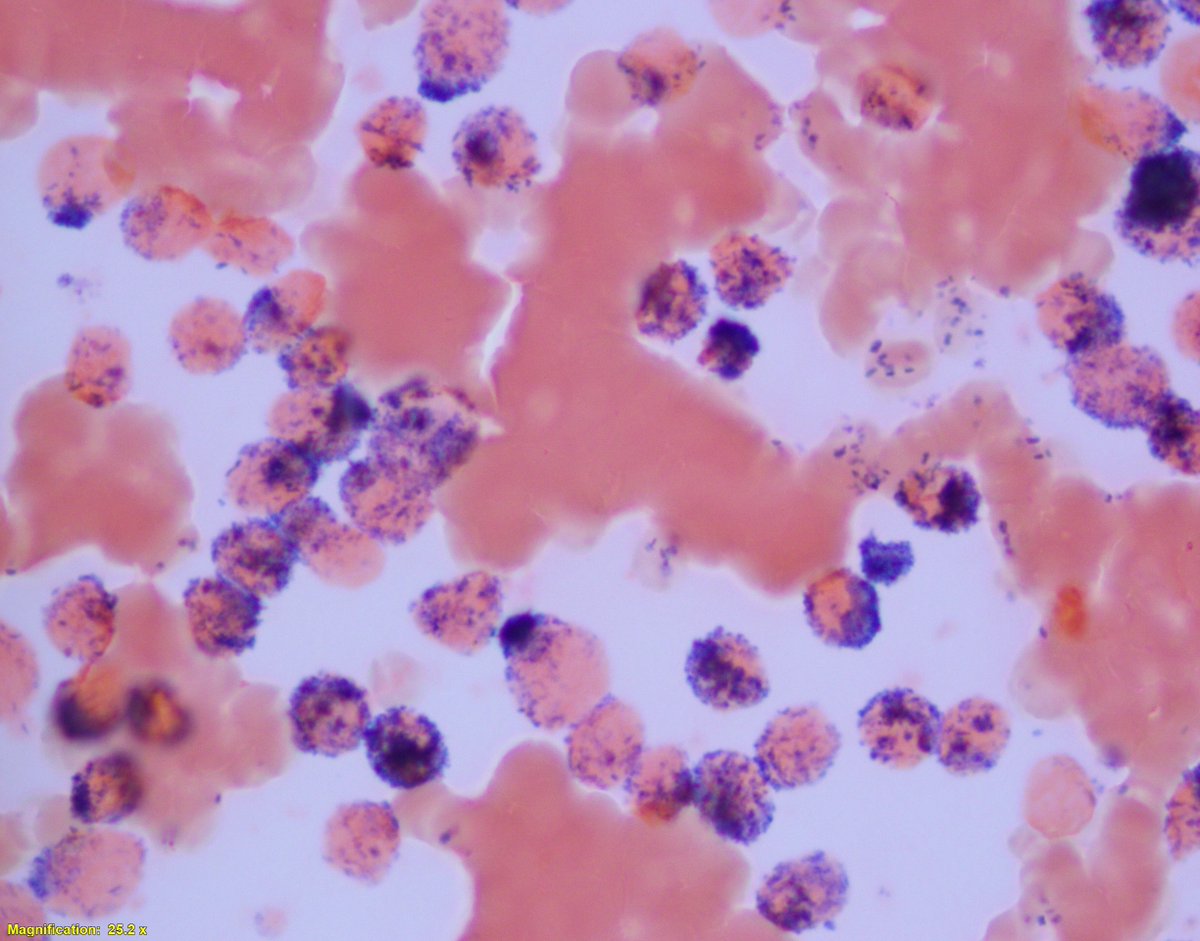
(1/5) AML with NPM1 mutation ⬇️
Characteristically prominent nuclear invaginations imparting a “cup-like” or “fish-mouth” morphology, with very strong MPO positivity 🔬
@KirillLyapichev @sanamloghavi
#hemepath #hemepathMDA #PathTwitter


Characteristically prominent nuclear invaginations imparting a “cup-like” or “fish-mouth” morphology, with very strong MPO positivity 🔬
@KirillLyapichev @sanamloghavi
#hemepath #hemepathMDA #PathTwitter


(2/5) Cytoplasmic staining of NPM1 protein by IHC is predictive of NPM1 mutations
#hemepath #hemepathMDA #PathTwitter

#hemepath #hemepathMDA #PathTwitter


(3/5) This is because NPM1 mutations cause loss of the nucleolar localization signal and addition of a nuclear export signal, leading to increased protein export from
the nucleus and aberrant accumulation in the cytoplasm
#hemepath #hemepathMDA #PathTwitter
the nucleus and aberrant accumulation in the cytoplasm
#hemepath #hemepathMDA #PathTwitter
Basics of #flowcytometry tweetorial!☺️
As promised @DrGeeONE @DrPayelMondal @siti_richardson @nusrat_xahra @seyma_buyucek @Gagandeepk5MD @RubyMughal2 @anjuthevirgo @anueru432 @kis_lorand @AlanPath @Pathology36 😁
1/11
#FlowCytomtery #HemePath #Flow #PathTwitter
As promised @DrGeeONE @DrPayelMondal @siti_richardson @nusrat_xahra @seyma_buyucek @Gagandeepk5MD @RubyMughal2 @anjuthevirgo @anueru432 @kis_lorand @AlanPath @Pathology36 😁
1/11
#FlowCytomtery #HemePath #Flow #PathTwitter
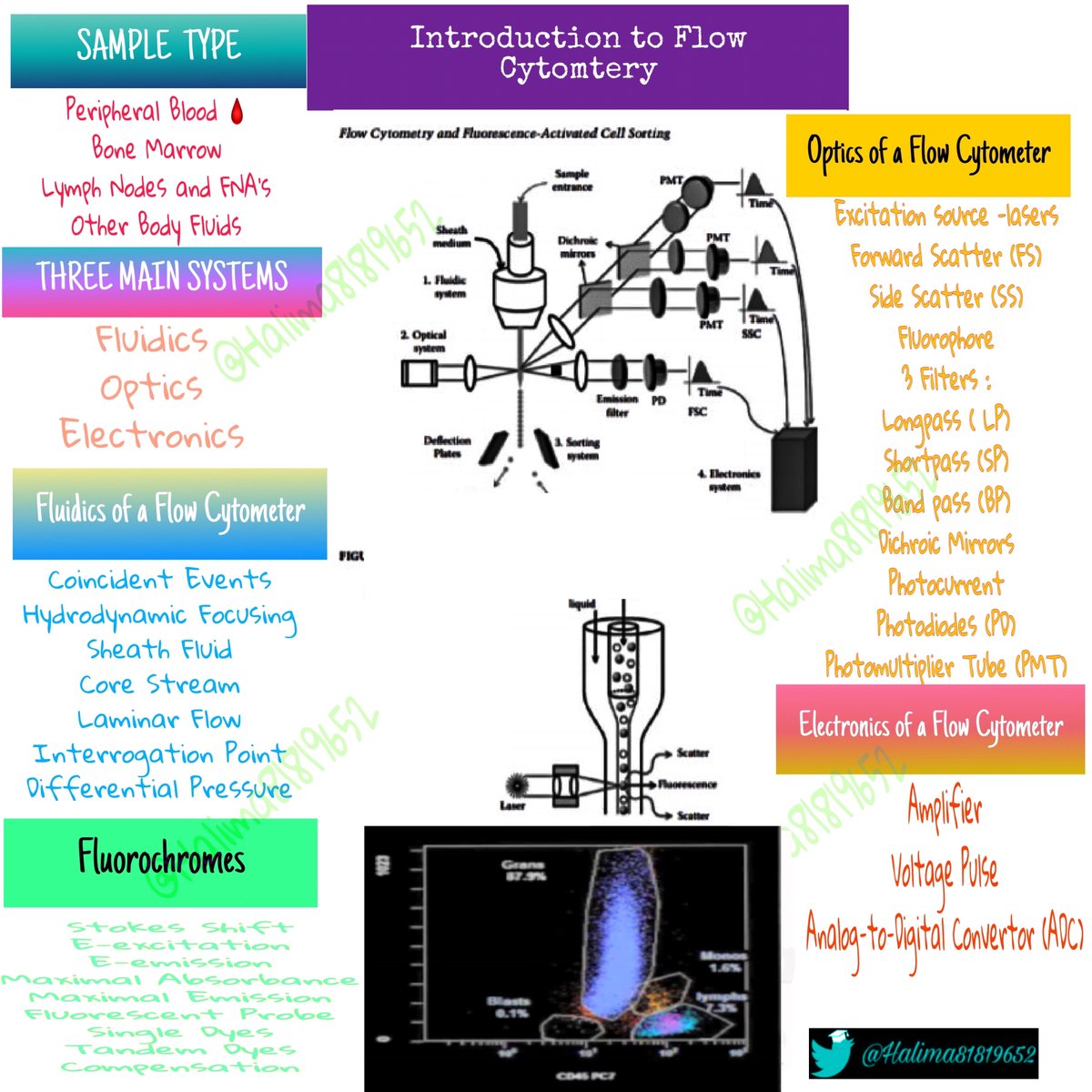
What is a Flow Cytometry?
💧Flow= fluid
💧Cyto= cells
💧Metry =measurement
Flow cytometry is a process of performing measurements on cells (or particles) that are in liquid suspension-multiple characteristics gets measured simultaneously as cell passes through light beam 2/11
💧Flow= fluid
💧Cyto= cells
💧Metry =measurement
Flow cytometry is a process of performing measurements on cells (or particles) that are in liquid suspension-multiple characteristics gets measured simultaneously as cell passes through light beam 2/11
A Brief History of Flow Cytometry:
The first invention of a coulter counter was in 1949 by Wallace H. Coulter- method for detecting and counting particles suspended in a fluid medium
Later named the Coulter principle.
3/11
#beckmancoulter
beckman.com/about-us/compa…
The first invention of a coulter counter was in 1949 by Wallace H. Coulter- method for detecting and counting particles suspended in a fluid medium
Later named the Coulter principle.
3/11
#beckmancoulter
beckman.com/about-us/compa…

Peripheral smear call thread #3: Lymphocytosis #hemepath @pathelective
First question when approaching a smear with lymphocytosis: is it reactive or neoplastic? Patient history can provide some clues (younger patient, symptoms of infection may favor reactive).
Peripheral smear call thread #2: Hemolysis #hemepath
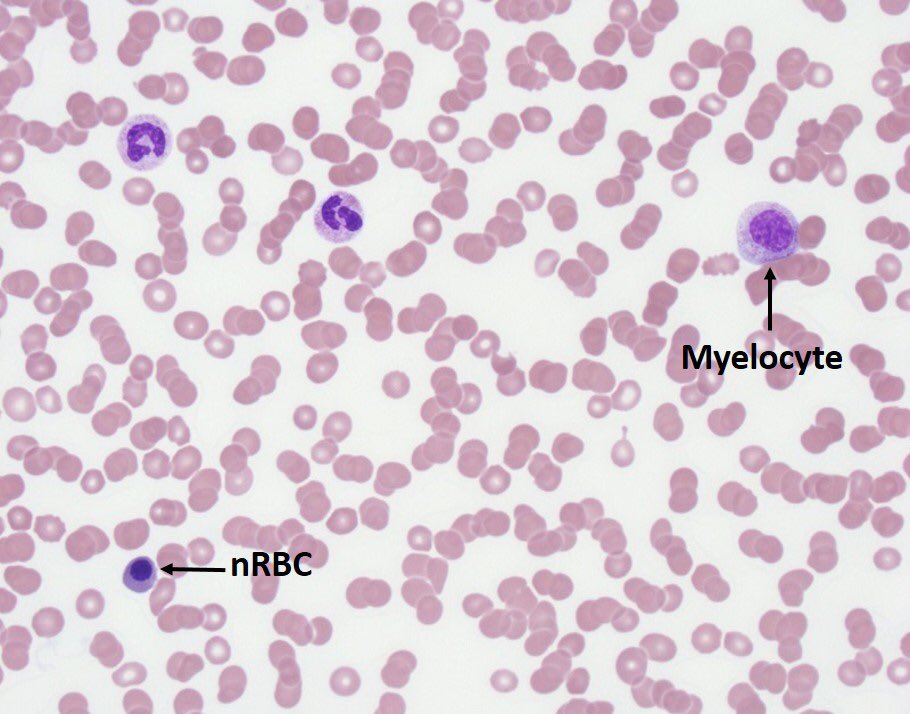
2/If the bone marrow is responding appropriately to hemolysis, there should be a reticulocyte response (& increased polychromasia on the smear). Lab abnormalities associated with hemolysis include increased LDH, increased unconjugated bili, and decreased haptoglobin.
3/Side note: these “hemolysis labs” are not totally specific. LDH is increased in other conditions where cell death / turnover is increased, including liver disease, malignancy, and MI.
1/For the path residents taking CP call for the first time this month, I thought I’d post a short series on things to look out for when you get called to look at a blood smear. First up: pancytopenia. #hemepath
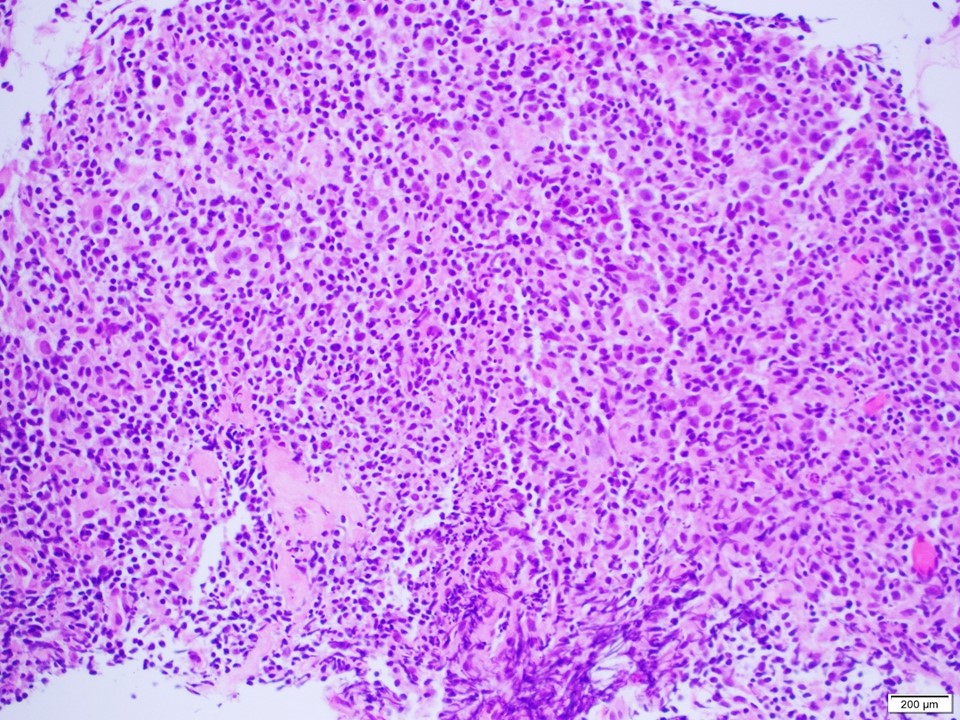
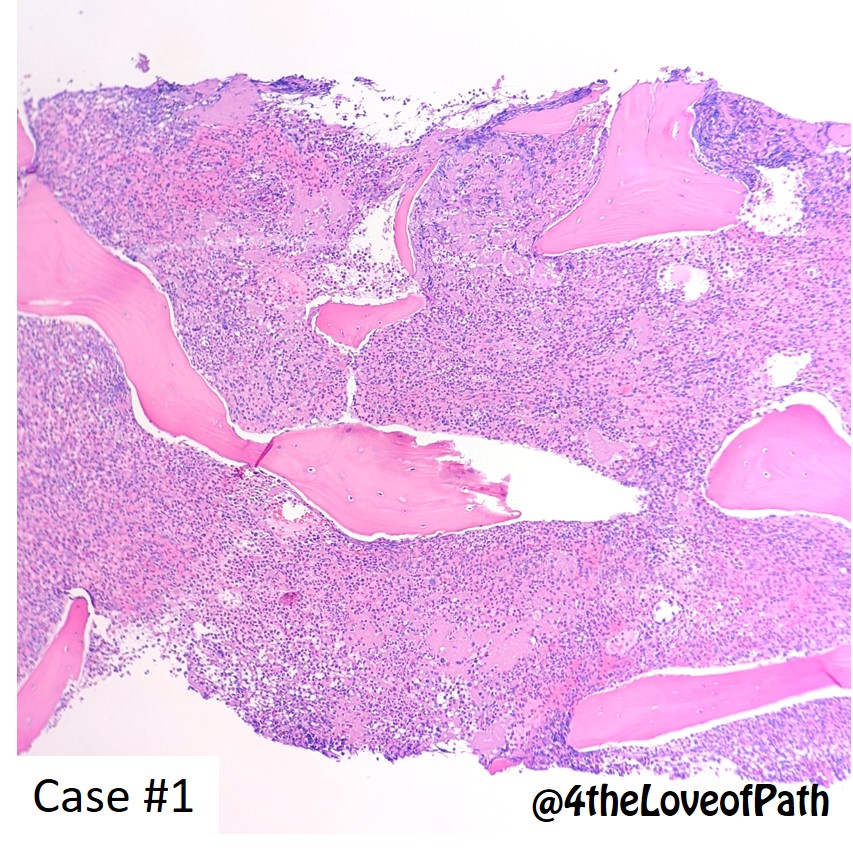
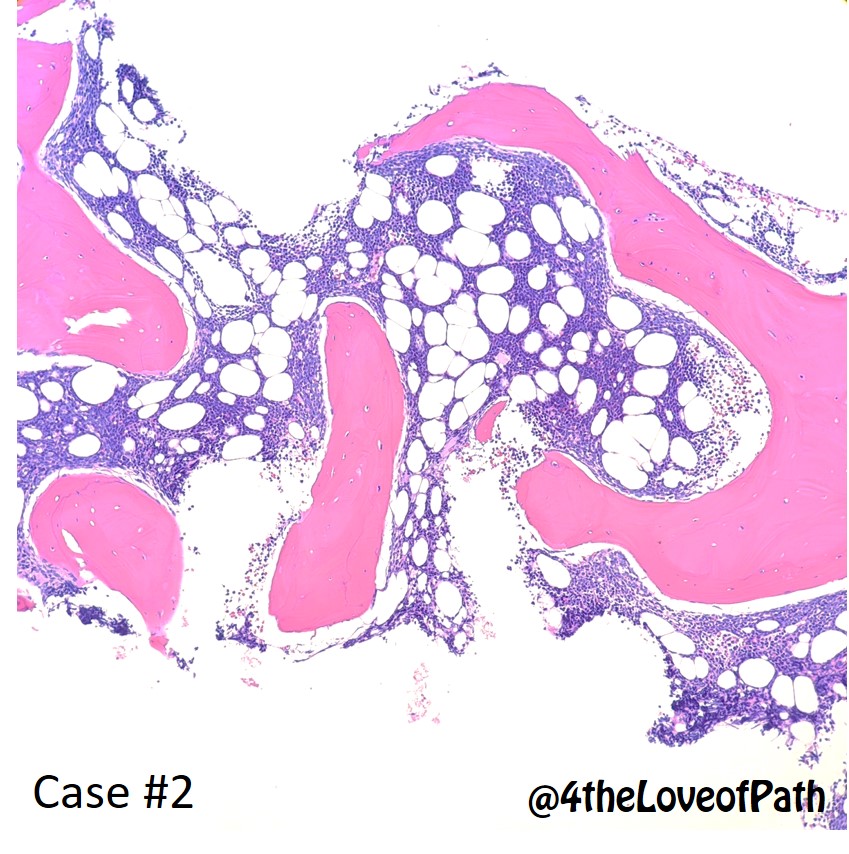
One of the many pearls that I learned from @ljmedeirosMD is:"The best time to learn, is after you know the diagnosis of a case, by going back to the slides and reading more about it".In this spirit, below are the answers of today's cases, with pictures #hemepath @KirillLyapichev
Case 1 : Marginal zone lymphoma
#hemepath #hemepathMDA #virtualhemepathMDA #virtualhemepath #virtualpath



#hemepath #hemepathMDA #virtualhemepathMDA #virtualhemepath #virtualpath
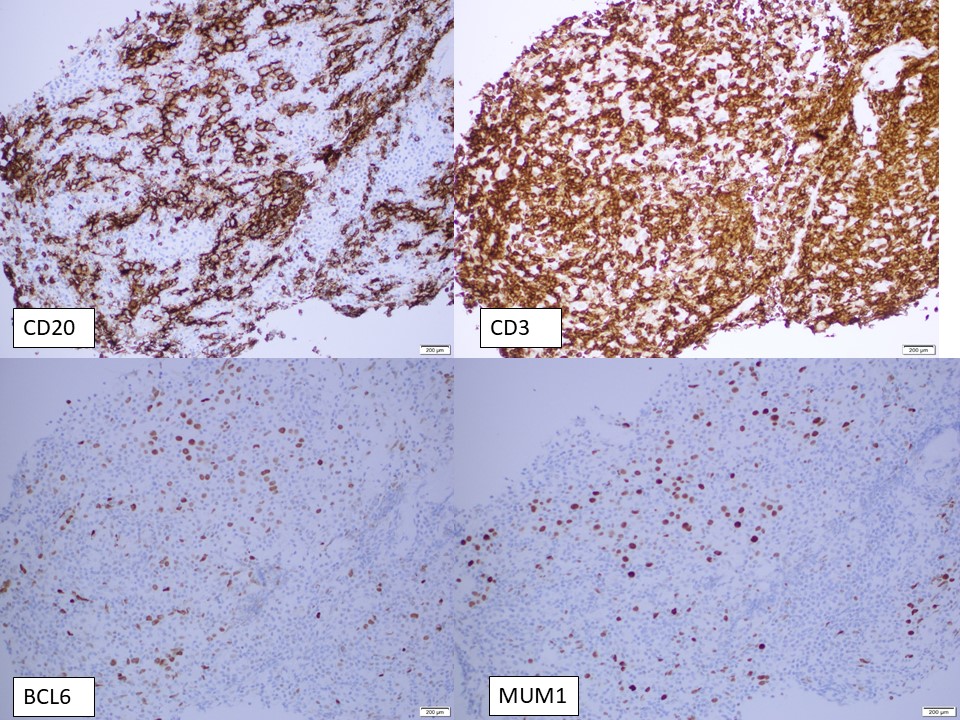
Case 2 : Diffuse large B-cell lymphoma, NGCB (with a T-cell rich background)
#hemepath #hemepathMDA #virtualhemepathMDA #virtualhemepath #virtualpath


#hemepath #hemepathMDA #virtualhemepathMDA #virtualhemepath #virtualpath
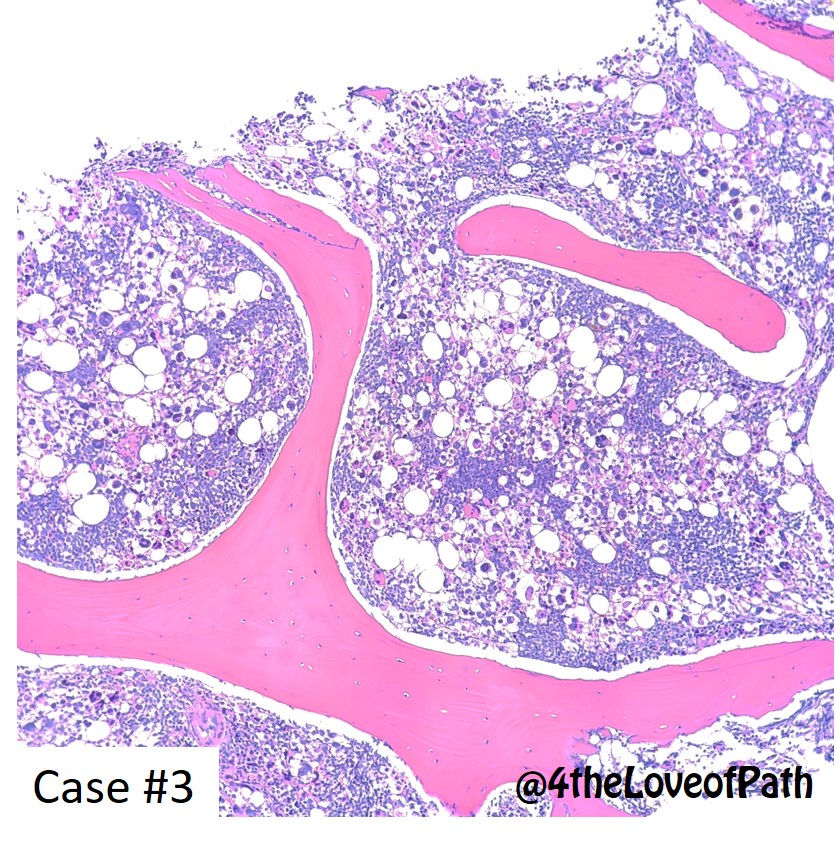
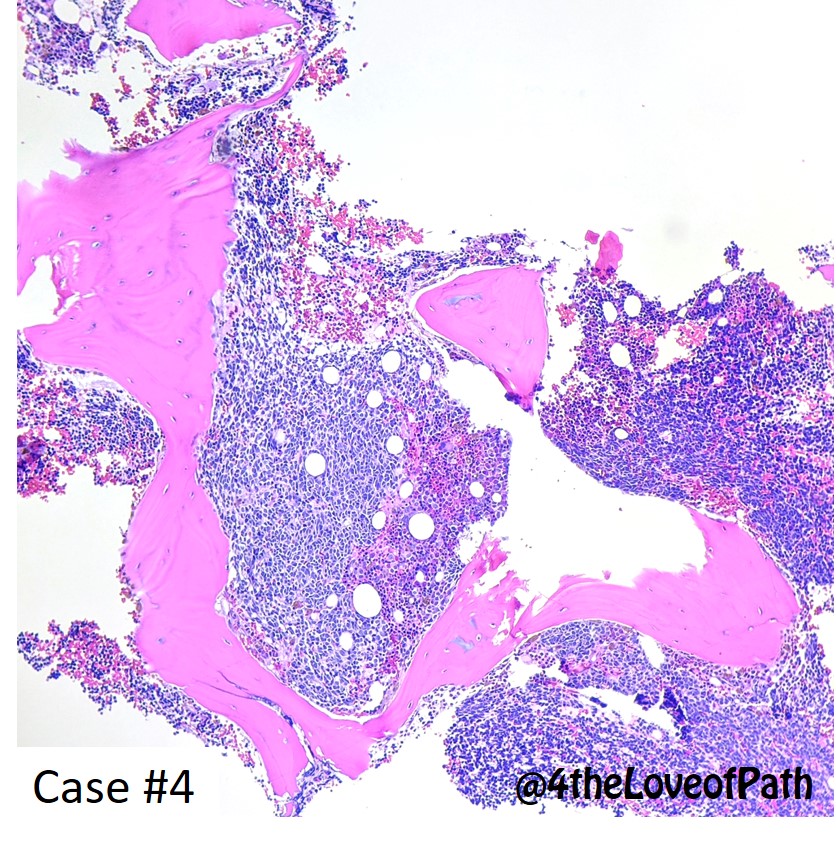
Instead of my normal #GTScase, I wanted to look at the morphology of pediatric bone marrows for #hemepath. Following @CArnold_GI ‘s advice, I am going to make these unknowns. Let's take a look! 👀 



#HematologyTweetstory 21: the “CD” nomenclature. Musical CDs may be obsolete (though I still have a lot of them from college days; Paul Simon’s “Graceland” wins for most listens). Communicating clearly about blood cell surface markers? Here to stay.🙂 @ASH_Hematology #hemepath/1 

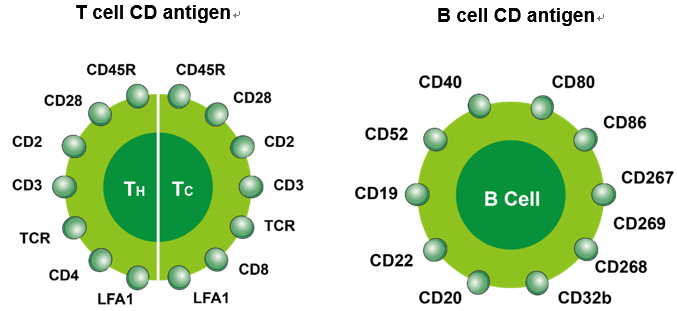
In the 1970s, German Georges Köhler & Argentinian-born César Milstein at @MRC_LMB fused myeloma cell lines w/ B cells to create immortal “hybridomas” that could produce specific monoclonal antibodies. Development of MoAbs led to a wave of discovery of cell-identifying markers./2 


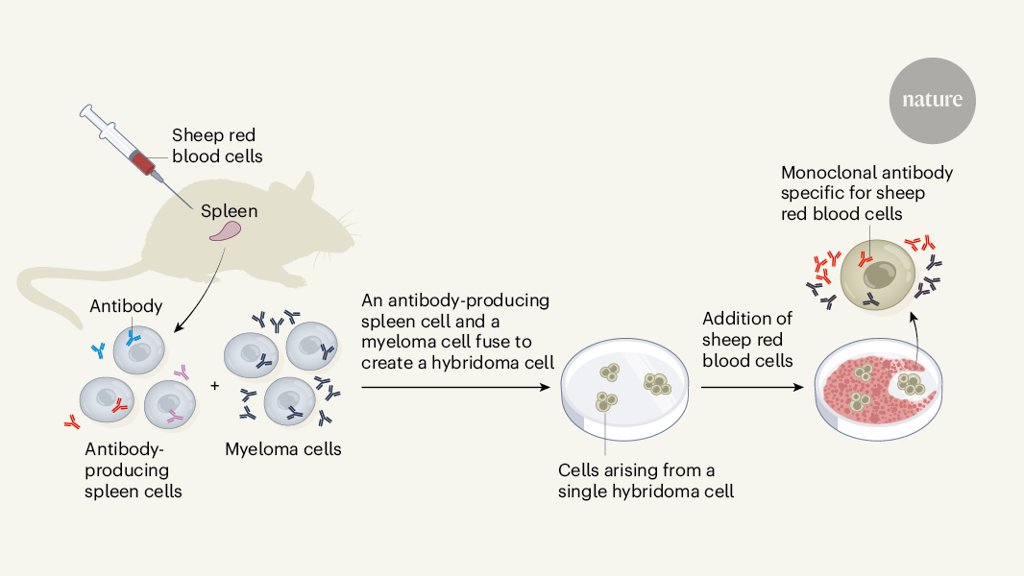
In the late 1970s & early 1980s, labs all across the world used this new #monoclonalantibody technology to move beyond morphology in cell identification. The same cell surface molecule identified by multiple laboratories was given different names. It got hard to read papers!/3 
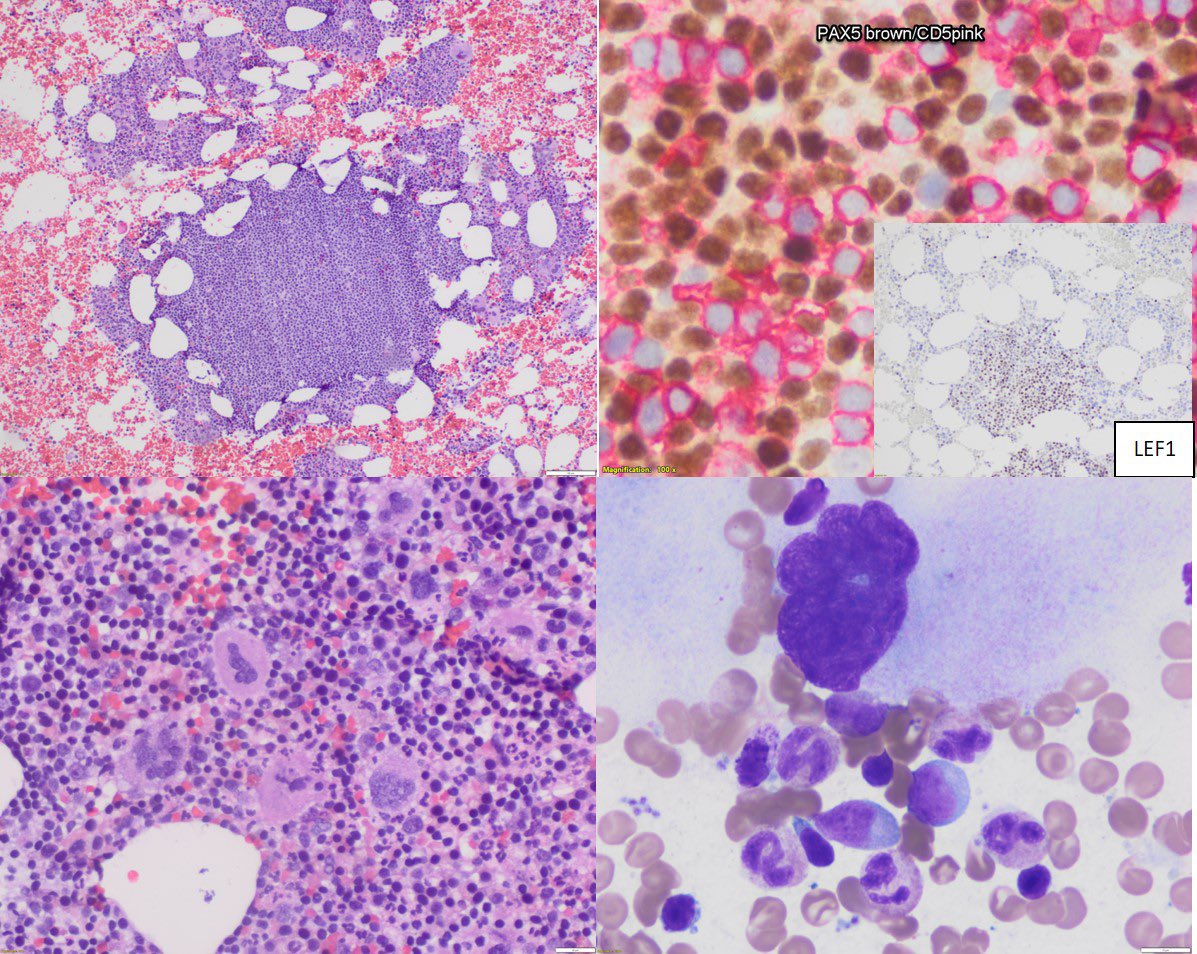
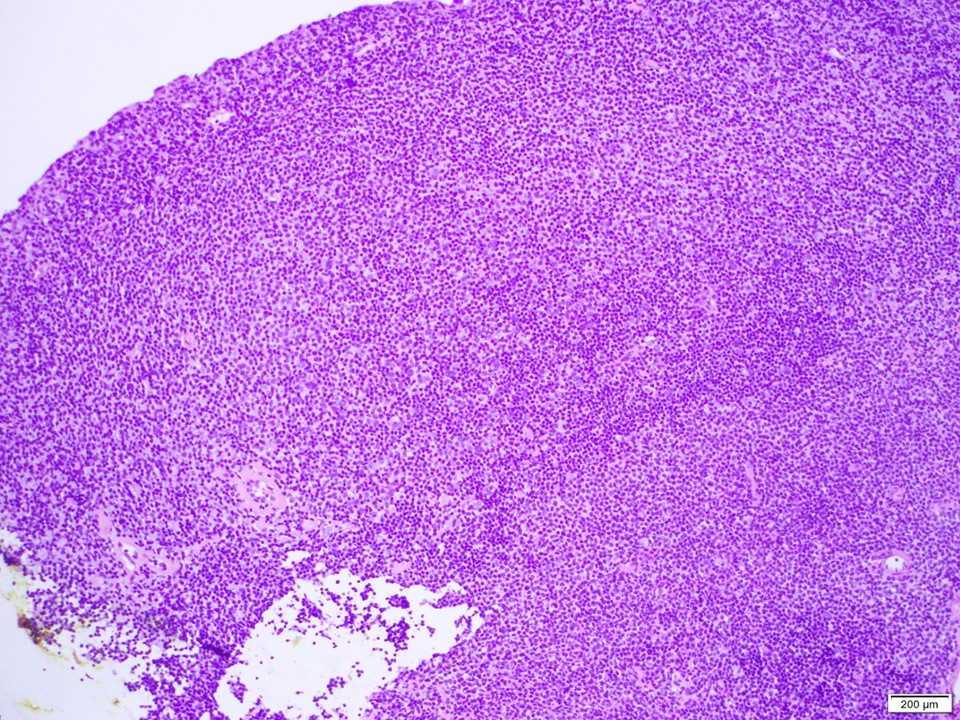
Young male, 30’s, came with an enlarged neck node
(Well that’s all the history that I got)
#pathology #HemePath #lymphnode


(Well that’s all the history that I got)
#pathology #HemePath #lymphnode