Discover and read the best of Twitter Threads about #SCCM2023
Most recents (24)
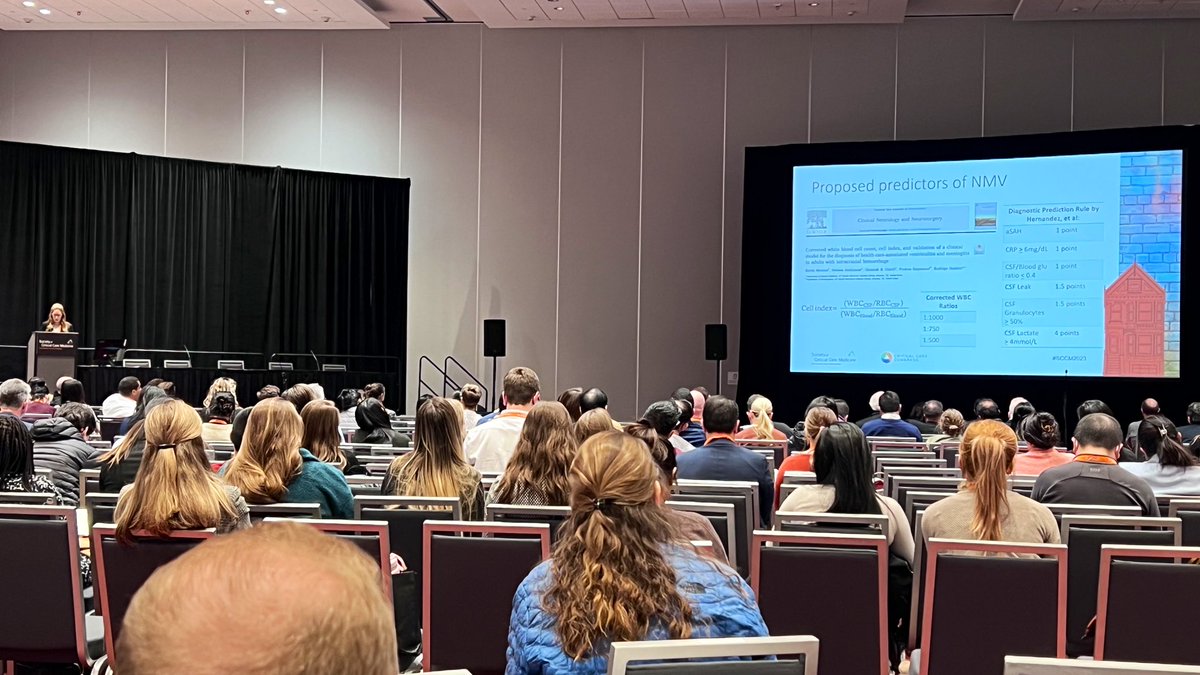
Cell index and corrected CSF WBC count can be used to generate a score where ≥6 indicates infection. There are challenges with regard to the sensitivity and specificity of this score.
@SarahE_NP provides updates on nosocomial meningitis and ventriculitis (NMV) #SCCM2023
@SarahE_NP provides updates on nosocomial meningitis and ventriculitis (NMV) #SCCM2023
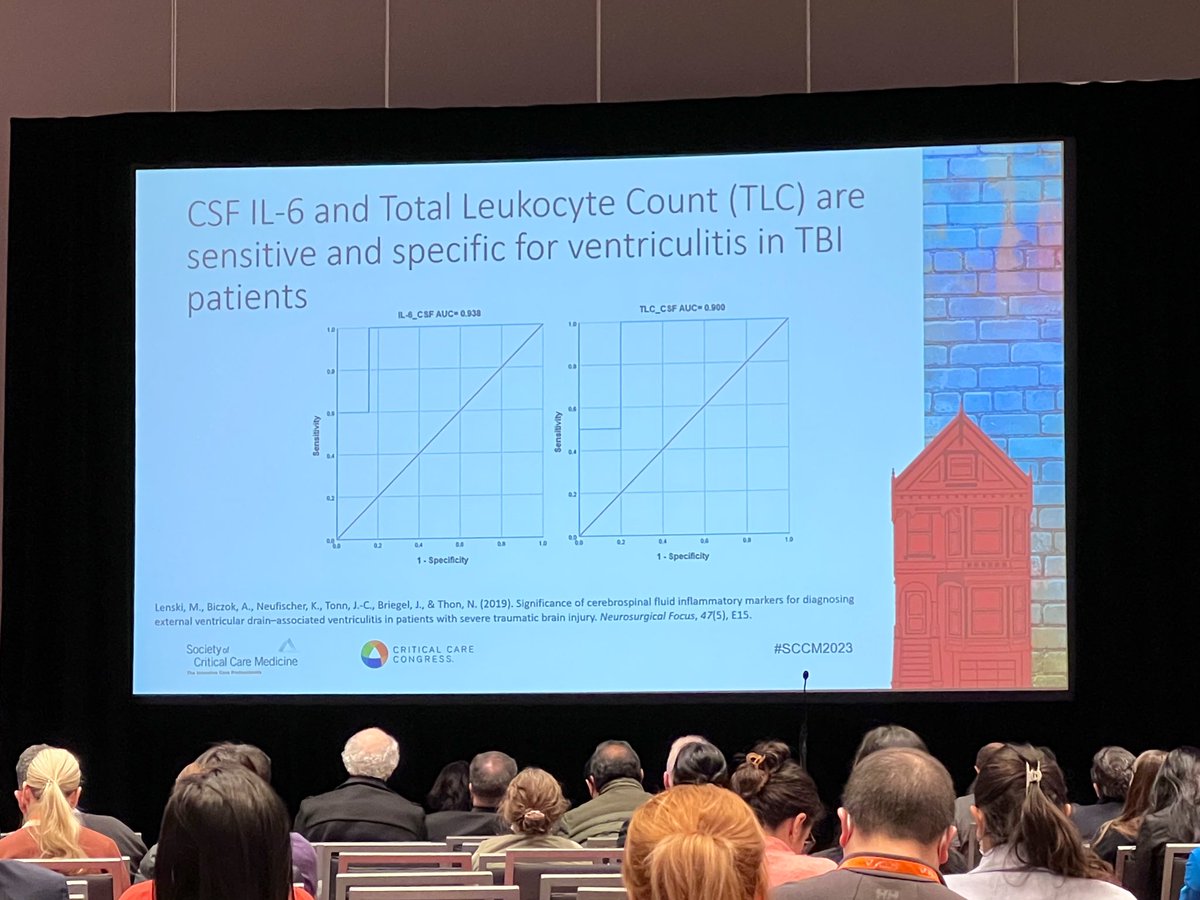
CSF IL-6 and total leukocyte count are sensitivity and specific for ventriculitis in traumatic brain injury patients #SCCM2023 
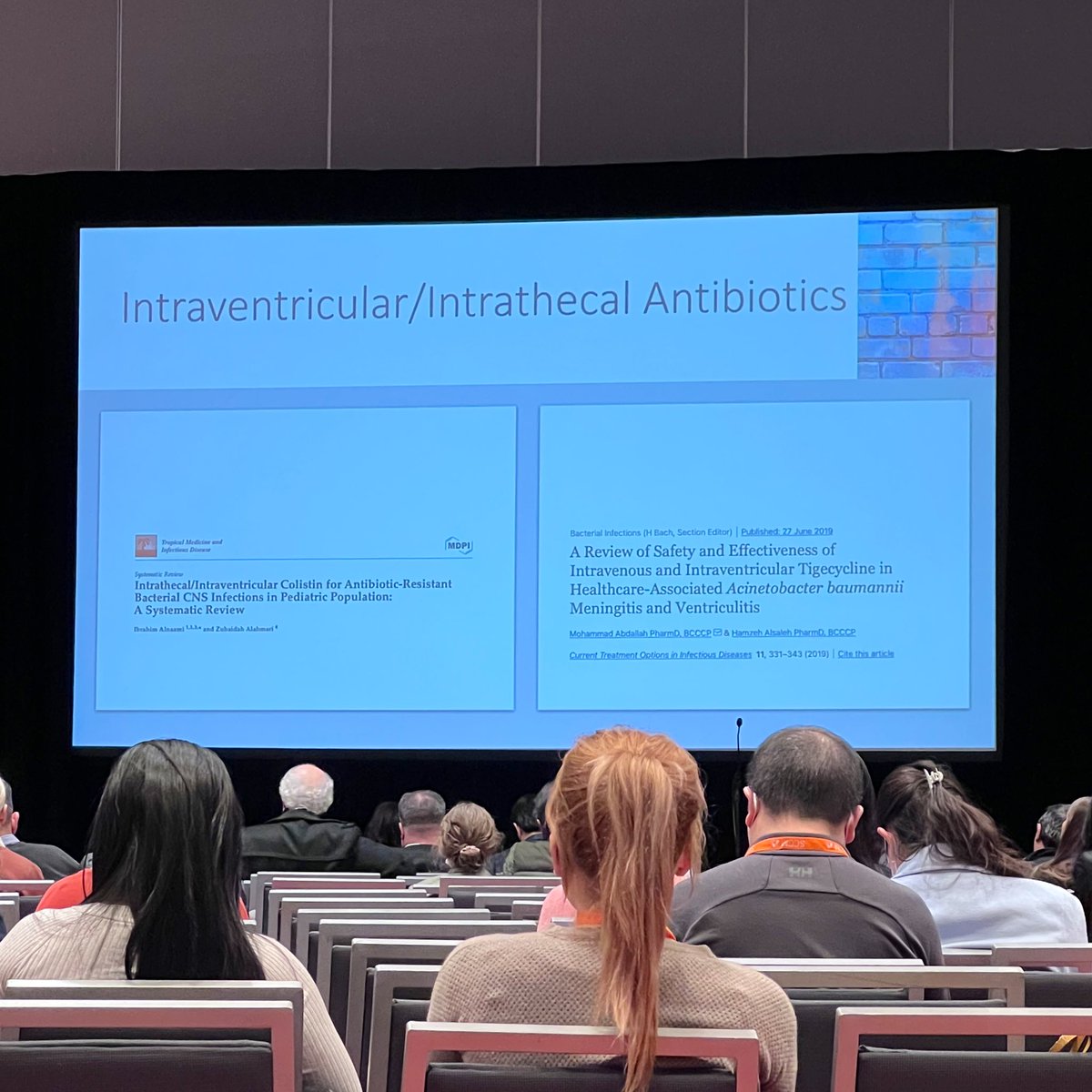
Intraventricular or intrathecal antibiotics should be considered in patients who do not respond to IV antibiotics or when resistant organisms are suspected #SCCM2023 
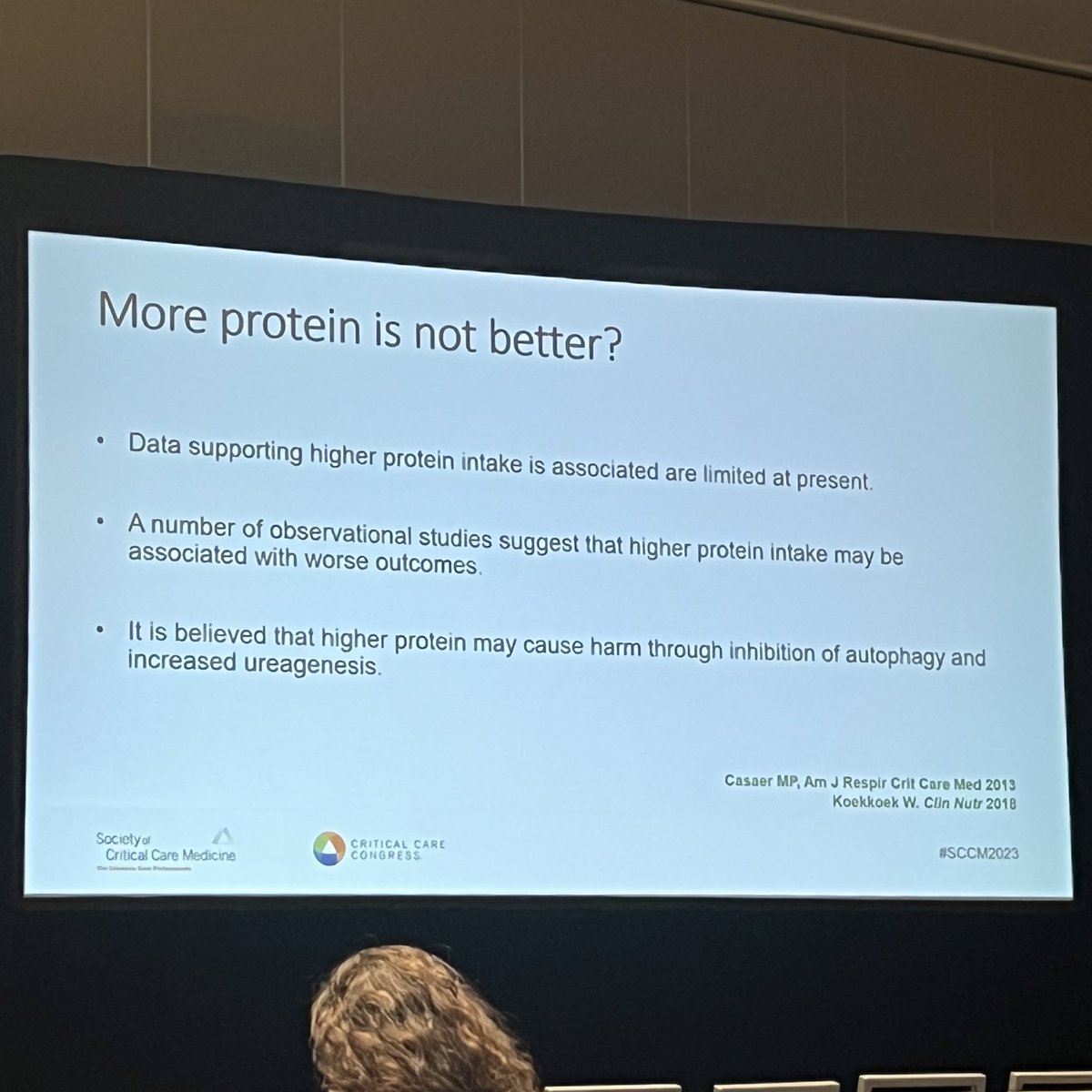
Arabi: negative nitrogen balance impacts various outcomes so it makes sense that we should give exogenous protein to compensate. #SCCM2023 #ICUNutrition 

High-dose, long duration beta-lactan therapy remains the mainstay of therapy for infective endocarditis. Gentamicin and rifampin-containing regimens are no longer necessary
#MeganHicks provides updates on endocarditis and cardiovascular infections #SCCM2023
#MeganHicks provides updates on endocarditis and cardiovascular infections #SCCM2023

STS RISK-E scoring system may be used to assist with determining surgical risk. Patients with cardiogenic shock or large mobile vegetations at eminent risk of mobilization require more emergent surgery #SCCM2023 

Repair of the tricuspid and mitral valves is preferred to replacement as there is potential survival benefit.
Replacement of the aortic valve is preferred #SCCM2023
Replacement of the aortic valve is preferred #SCCM2023

Questions Patel will answer today. Situations where we might pause before giving nutrition. #SCCM2023 #ICUNutrition 

Rapid diagnostics may provide faster time to targeted therapy in HAP/VAP infections. Specificity can be as high as 99% with sensitivity to 100% in either BAL or sputum cultures.
@ScottMicek reviews updates to HAP/VAP therapy and the impacts on stewardship #SCCM2023 @SCCM_CPP
@ScottMicek reviews updates to HAP/VAP therapy and the impacts on stewardship #SCCM2023 @SCCM_CPP

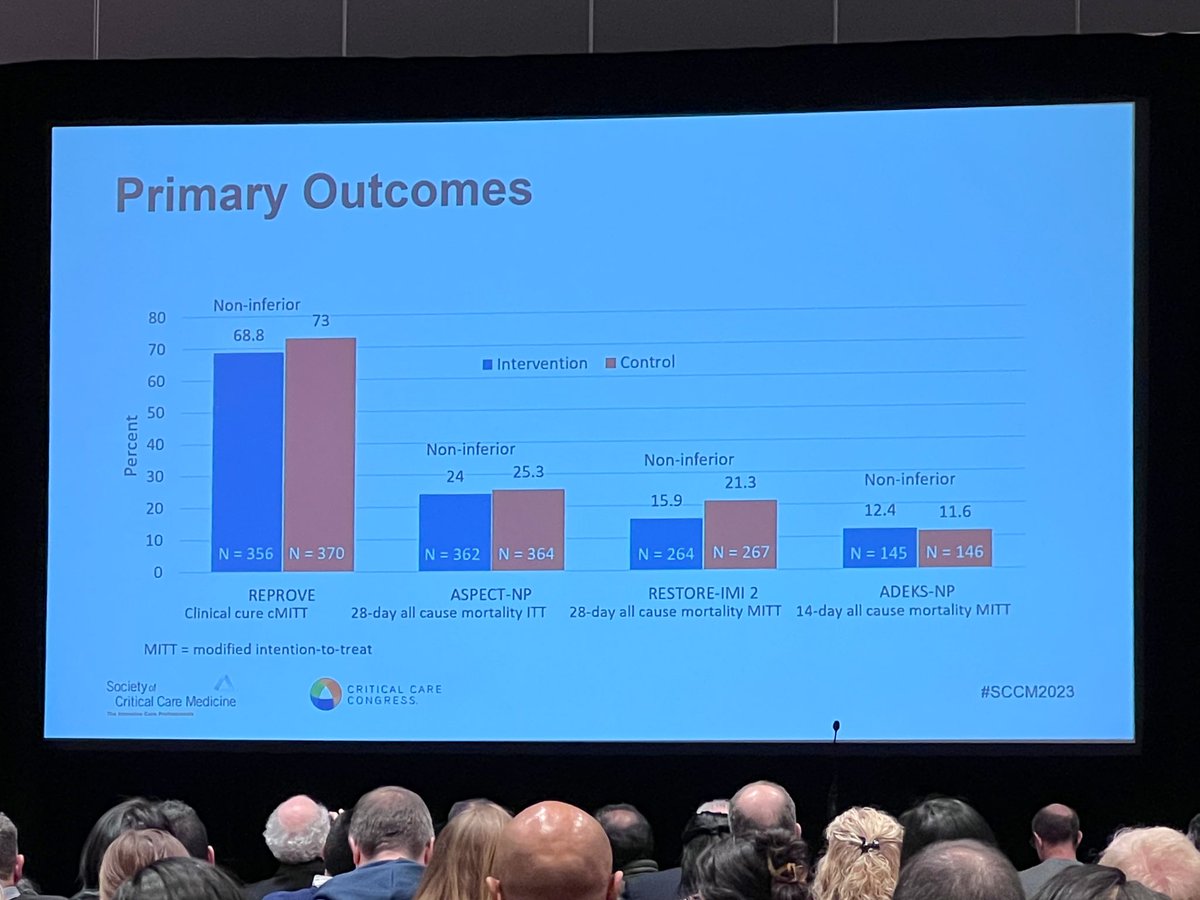
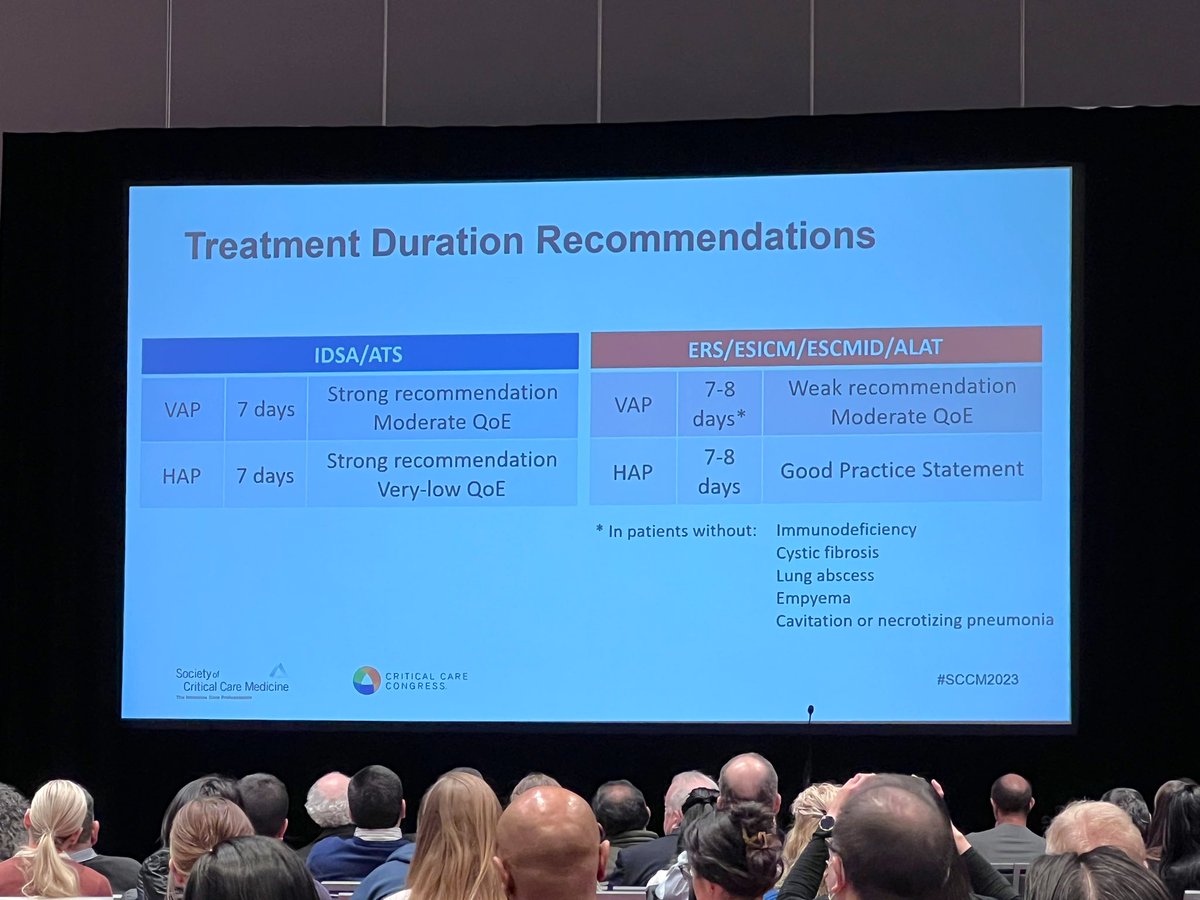
Multiple studies have been published with new antibiotics since the most recent HAP/VAP guidelines were published. These antibiotics were shown as non-inferior in their clinical trials which may result in many alternative options listed in the next guideline update #SCCM2023 


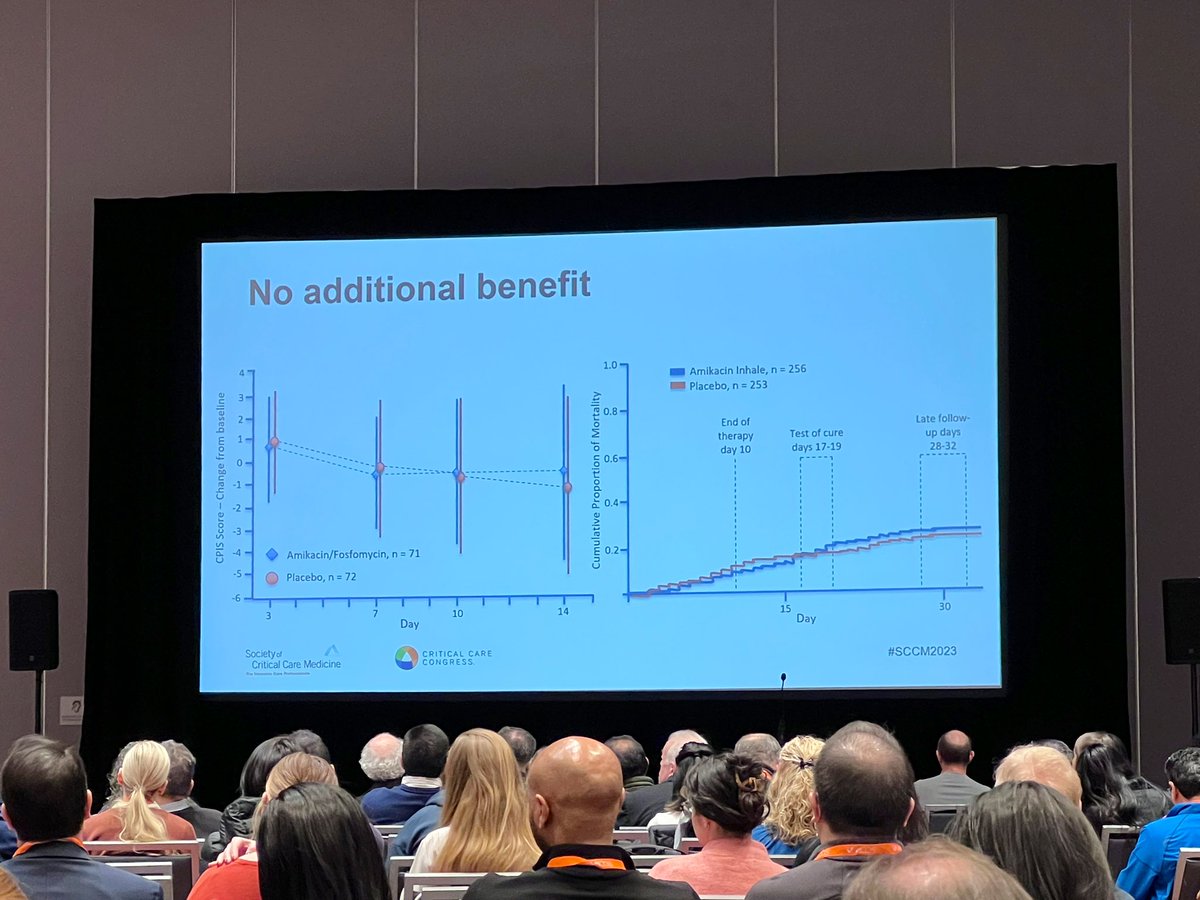
No additional benefit was observed by adding inhaled aminoglycosides in HAP/VAP infections.
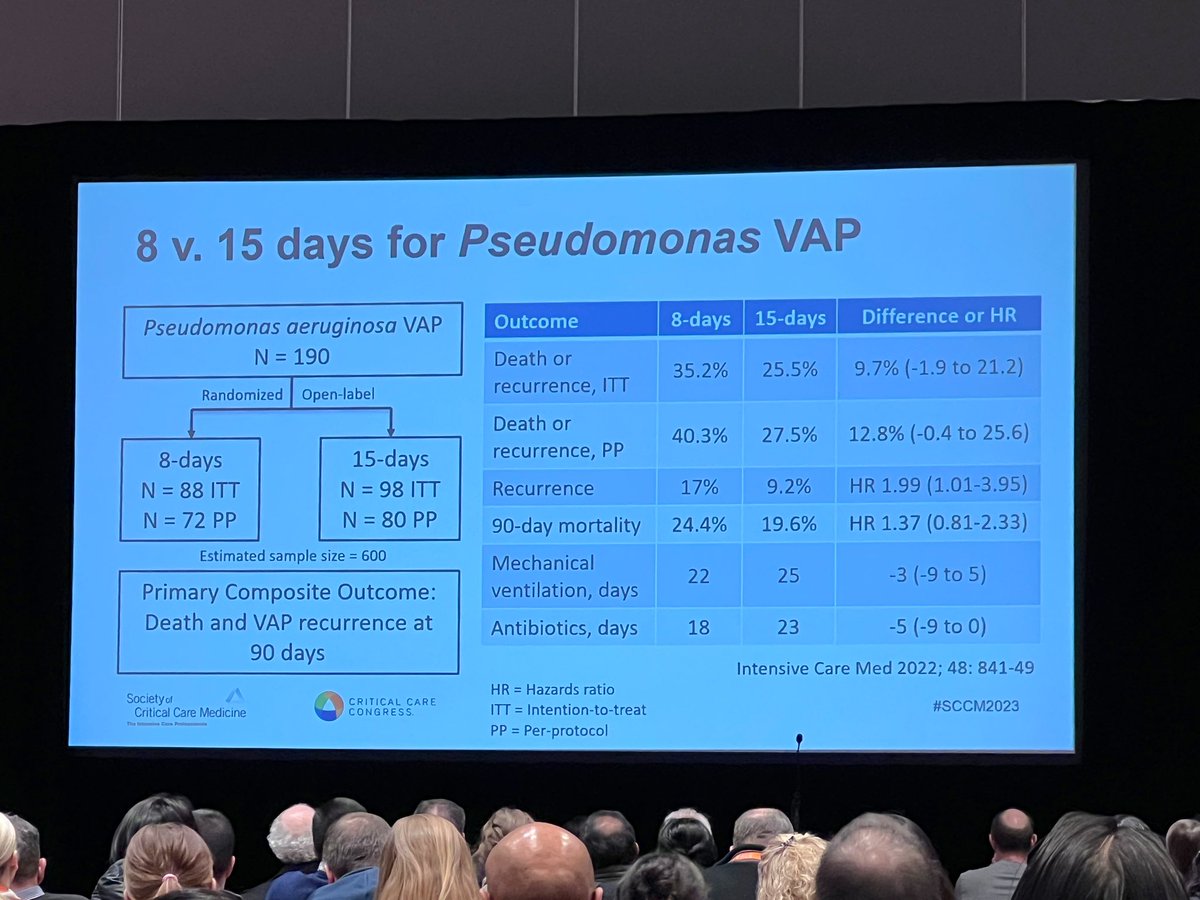
Updates to the Chastre study from the early 2000s failed to show non-inferiority due to recruitment in 8 vs 15 days of treatment for non-fermenter bacterial HAP/VAP infections #SCCM2023


Updates to the Chastre study from the early 2000s failed to show non-inferiority due to recruitment in 8 vs 15 days of treatment for non-fermenter bacterial HAP/VAP infections #SCCM2023
@NileshMehtaMD up next to discuss what’s new in #ICUNutrition guidelines and how he has interpreted them. #SCCM2023 

Mehta: guidelines must have clinical context. #SCCM2023 #ICUNutrition
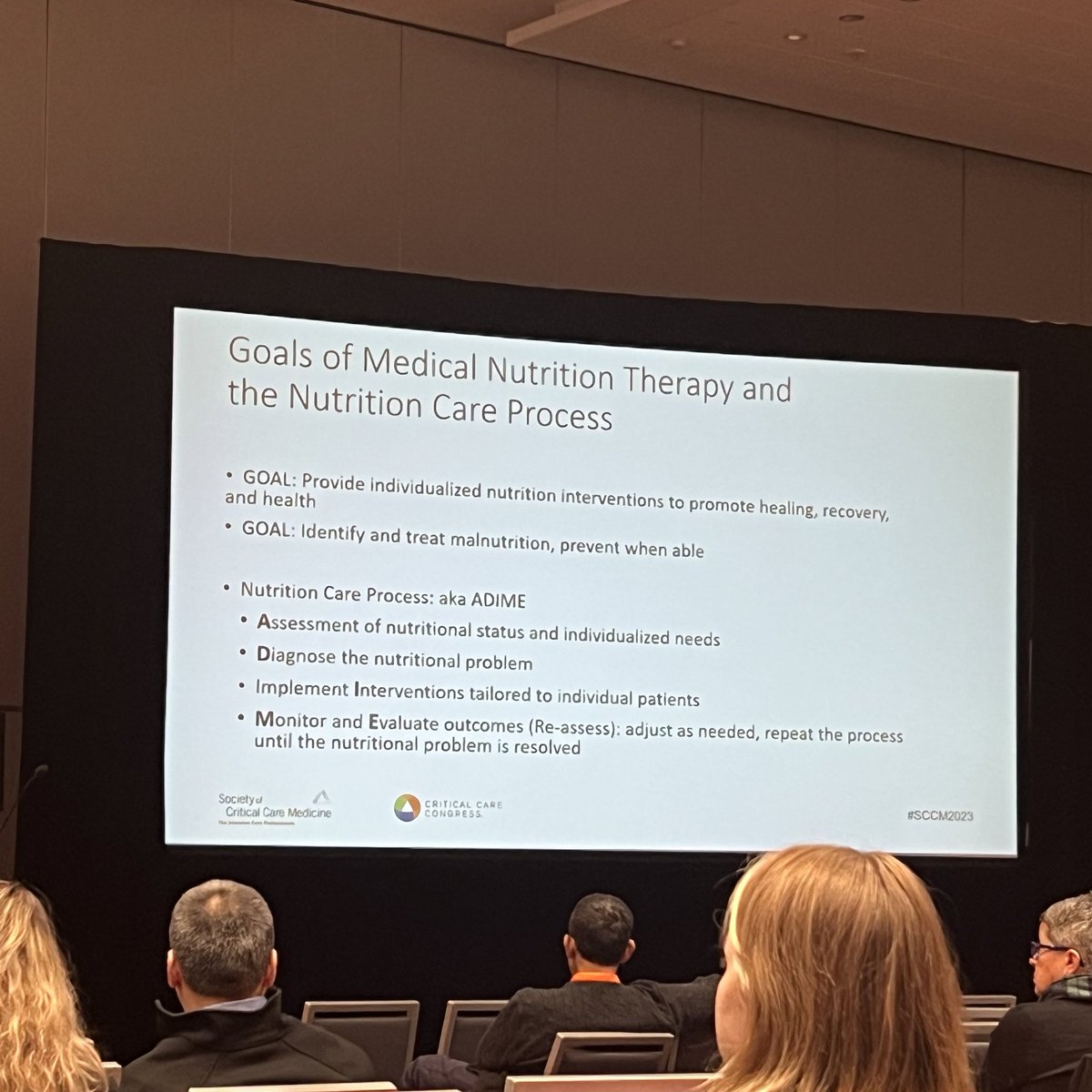
Sharon Irving, CRNP, MSN, PhD, PNP starting off the afternoon nutrition lecture with why we call it NUTRITION THERAPY. #SCCM2023 #ICUNutrition 

Lots of metabolic changes in critical illness that prevent adequate prevention on nutrition. #SCCM2023 #ICUNutrition 

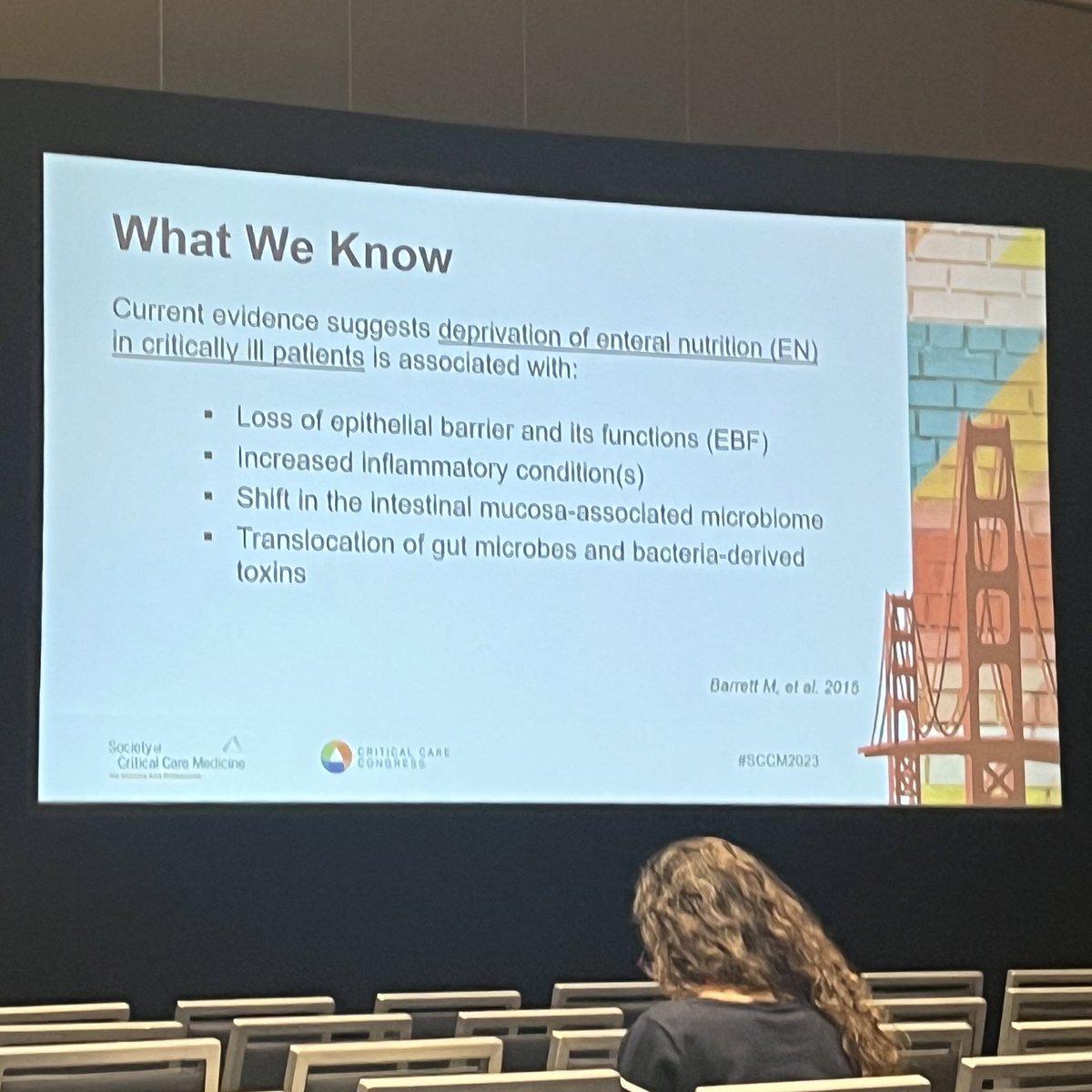
Irving: depriving the gut of EN causes problems. Failing to maintain gut mucosa and microbiome causes shifts in homeostasis. #SCCM2023 #ICUNutrition 
Yes! @gretchemaben now discussing the POSITIVES of social media. We must be intentional with how we use it. #SCCM2023 

@SheilaMyatra beginning the morning plenary lecture showing a major disparity in care related to staffing btwn US and India, her hospital having 42,000 pts/yr with 200 faculty. #SCCM2023 

Reasons to give vs not to give fluids. #SCCM2023 

Allan Walkey on atrial fibrillation in ICU (#SCCM2023)
Arrigo 2015: cardioversion for secondary A-fib in ICU rarely works (43% remains sinus at 1hr, 23% at 24hr). Diltiazem was more effective at rate control than amio or digoxin.
Arrigo 2015: cardioversion for secondary A-fib in ICU rarely works (43% remains sinus at 1hr, 23% at 24hr). Diltiazem was more effective at rate control than amio or digoxin.
Walkey 2016: Afib in sepsis? Association on outcome of BB vs CCB, BB vs digoxin, BB vs amiodarone compared. BB had slightly lower mortality than CCB.
Bosch 2021: BB achieved more HR reduction than amiodarone, CCB, and dioxin at 1hr (CCB was highest at 6 hours).
Bosch 2021: BB achieved more HR reduction than amiodarone, CCB, and dioxin at 1hr (CCB was highest at 6 hours).
Davey 2005: magnesium was about as effective at rhythm control as amiodarone.
Remember untreated infection, volume status, presence of beta agonists.
Law 2022: phenylephrine vs norepinephrine for shock? HR difference was only about 2-6 only, even in the subgroup with RVR.
Remember untreated infection, volume status, presence of beta agonists.
Law 2022: phenylephrine vs norepinephrine for shock? HR difference was only about 2-6 only, even in the subgroup with RVR.
What are the goals of Medical Nutrition Therapy? Preventing #malnutrition. Since most trauma pts are young & healthy, we have a big opportunity to prevent malnutrition in this population. #SCCM2023 #ICUNutrition 
Kevin Betthauser on empiric anaerobic antibiotics in the ICU (#SCCM2023)
gut dysbiosis common in ICU patients. Gut integrity degrades. Reduction in firmicutes and bacteriodetes, increase in proteobacteria. Less commensals, more opportunistic infections.
gut dysbiosis common in ICU patients. Gut integrity degrades. Reduction in firmicutes and bacteriodetes, increase in proteobacteria. Less commensals, more opportunistic infections.
In animal models, depletion of anaerobes increases susceptibility to bacterial PNA, lung injury, mortality. Preserving anaerobes by SDD associated with less VAP, less mortality. (Szychowiak 2022, Hammond 2022)
ATS/IDSA 2019 CAP guidelines: suggest not routinely covering aspiration pneumonia for anaerobes. Modern syndromes typically CAP organisms, not anaerobic. Kioka 2017, Marrin-Corral 2021, Brummitt 2022 - show anaerobic coverage is downtrending over past five years.
Richard Branson on bronchodilators (#SCCM2023)
clear standard of care for bronchoconstriction, but mostly used for hypoxemic disease because it "can't hurt". Ehrmann 2013 European survey found 95% used them routinely in mechanically ventilated
clear standard of care for bronchoconstriction, but mostly used for hypoxemic disease because it "can't hurt". Ehrmann 2013 European survey found 95% used them routinely in mechanically ventilated
BALTI trial: IV B-agonists for ALI improved resolution of alveolar edema and survival
Perkins 2014: salmeterol didn't improve ALI
BALTI-2: salbutamol, stopped for harm
Perkins 2014: salmeterol didn't improve ALI
BALTI-2: salbutamol, stopped for harm
Routine nebs create significant workload and disposable equipment burden
Device types vary by efficiency, but we use so much drug it likely doesn't matter - it gets delivered.
Device types vary by efficiency, but we use so much drug it likely doesn't matter - it gets delivered.
4 RCTs published in the last few hours you can’t miss if you work with critically ill patients:
#1 Fluids in septic shock
#2 Mobilisation and long-term cognitive impairment
#3 NIV for extubation of obese patients
#4 Nutrition before extubation
A thread 🧵👇
#FOAMcc #SCCM2023
#1 Fluids in septic shock
#2 Mobilisation and long-term cognitive impairment
#3 NIV for extubation of obese patients
#4 Nutrition before extubation
A thread 🧵👇
#FOAMcc #SCCM2023
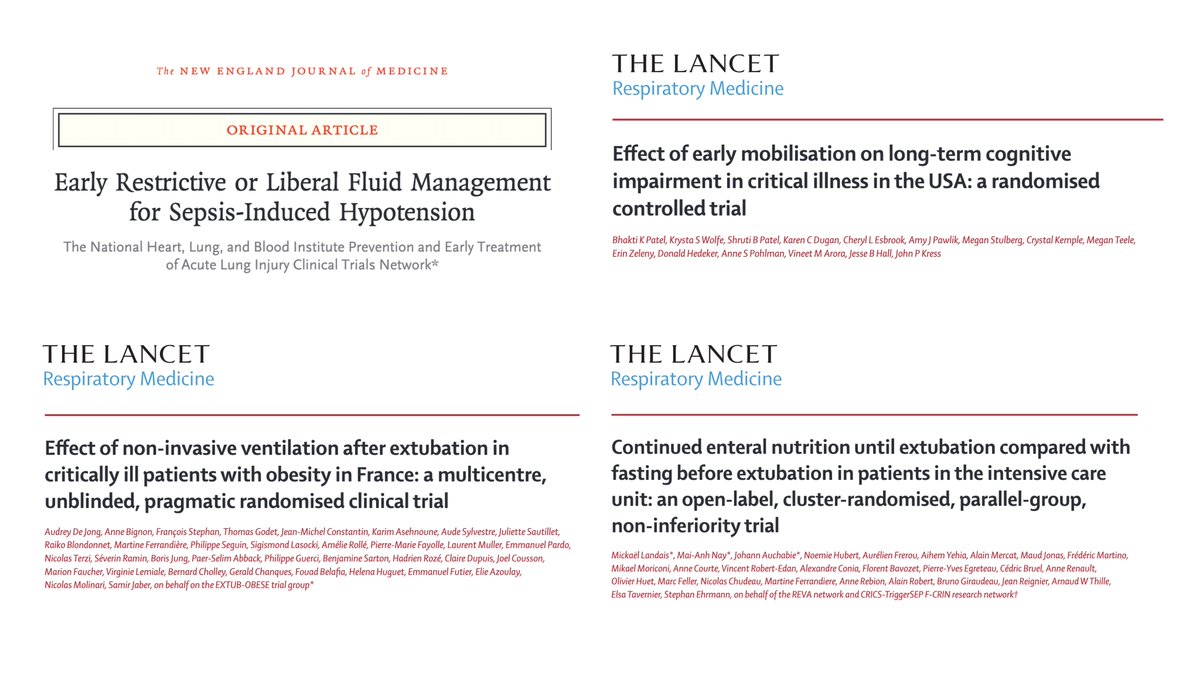
#1
#CLOVERStrial compared a restrictive fluid strategy (with early vasopressors) to a liberal one in septic shock patients.
➡️ Restrictive fluid strategy (with early vasopressors) did not result in significantly lower (or higher) mortality
🔗 nej.md/3CWSXBA
#FOAMcc
#CLOVERStrial compared a restrictive fluid strategy (with early vasopressors) to a liberal one in septic shock patients.
➡️ Restrictive fluid strategy (with early vasopressors) did not result in significantly lower (or higher) mortality
🔗 nej.md/3CWSXBA
#FOAMcc

#2
What’s the effect of early mobilisation on long-term cognitive impairment in ICU survivors after mechanical ventilation?
➡️ Early mobilisation improved long-term cognitive impairment at 1 y (24% vs 43%) but increased adverse events (6%)
🔗 bit.ly/3CYIZQ7
#FOAMcc
What’s the effect of early mobilisation on long-term cognitive impairment in ICU survivors after mechanical ventilation?
➡️ Early mobilisation improved long-term cognitive impairment at 1 y (24% vs 43%) but increased adverse events (6%)
🔗 bit.ly/3CYIZQ7
#FOAMcc

Shelby Yaceczko on nutrition in critical illness + obesity (#SCCM2023)
malnourished inpatients have 3.4x risk of in-hospital death, but only 2.7% of patients with coded malnutrition actually receive enteral nutrition in the hospital.
malnourished inpatients have 3.4x risk of in-hospital death, but only 2.7% of patients with coded malnutrition actually receive enteral nutrition in the hospital.
malnutrition in ICU associated with length of stay, higher cost of care. ASPEN did a value analysis, shows nutrition support saves money (projected $222 million yearly Medicare savings).
ASPEN 2021 guidelines:
1. How much should you give? No difference between high and low levels of nutrition. Give 12-25 kcal/kg BW in first 7-10 days of ICU stay. (Old recs: depended on disease and malnutrition risk.)
1. How much should you give? No difference between high and low levels of nutrition. Give 12-25 kcal/kg BW in first 7-10 days of ICU stay. (Old recs: depended on disease and malnutrition risk.)
My final #SCCM2023 tweetucation session for today is “Late-Breaking Studies Affecting Patient Outcomes”!
First we have “Continued Enteral Nutrition Until Extubation Compared to Fasting Prior to Extubation in the Intensive Care Unit: A Clustered Randomized Trial” with Stephan Ehrmann (@stephanehrmann)! #SCCM2023 

Nearly all ICUs impose some form of fasting before extubation, but this time seems to be decreasing. #SCCM2023 

Bethany Shoulders on Pharmacotherapy in critical illness + obesity (#SCCM2023)
Absorption: may be reduced both enteral and subq
Distribution: Increased
Metabolism: may decrease
Excretion: Often increased
Absorption: may be reduced both enteral and subq
Distribution: Increased
Metabolism: may decrease
Excretion: Often increased
B-lactams (inc. cephalosporins, meropenem, pip/tazo): good data on impact of obesity. more treatment failure, longer hospitalizations, risk of cefepime neurotoxicity. Use monitoring! Target 40-100% free time >MIC.
Anticoagulation (enoxaparin, heparin): Use higher dose for prophylaxis. No dose cap for weight-based dose of enoxaparin. May not need heparin dose increase unless BMI >50. For therapeutic heparin, slight preference to adjusted BW + no cap.
Sara A Hennessy on managing ICU devices in obesity (#SCCM2023)
BP cuffs taken with too-small cuffs significantly higher. Should be 80% of upper arm circumference, width should be 40% of length. Large cuffs may still be poor fit, eg too long (obese arms aren't longer), and arms are "inverted cones" not cylinders.
Try an appropriate cuff on forearm, hold forearm at level of heart; hoses should exit over radial artery. Will vary by 7-15mmHg from upper arm.
Sam Galvagno on airway management in obesity (#SCCM2023)
oxygenation normal, but poor reserve - low compliance, compression of small airways at bases. ERV, TLC, FRC reduced.
P's of airways in obesity: Prediction, Positioning, Preox, Performance, Postintubation management
oxygenation normal, but poor reserve - low compliance, compression of small airways at bases. ERV, TLC, FRC reduced.
P's of airways in obesity: Prediction, Positioning, Preox, Performance, Postintubation management
Prediction: obesity = difficult mask, but less clear association with difficult intubation.
Position: sniffing position helps everyone. Ramped position helps the obese - also makes it easier to insert laryngoscope handle.
Position: sniffing position helps everyone. Ramped position helps the obese - also makes it easier to insert laryngoscope handle.
Modified ramped position can be done with a pyramid-shaped pillow.
Fastest method is just put them in reverse Trendelenburg - better than just elevating head.
Fastest method is just put them in reverse Trendelenburg - better than just elevating head.
Patient enrollment #SCCM2023 
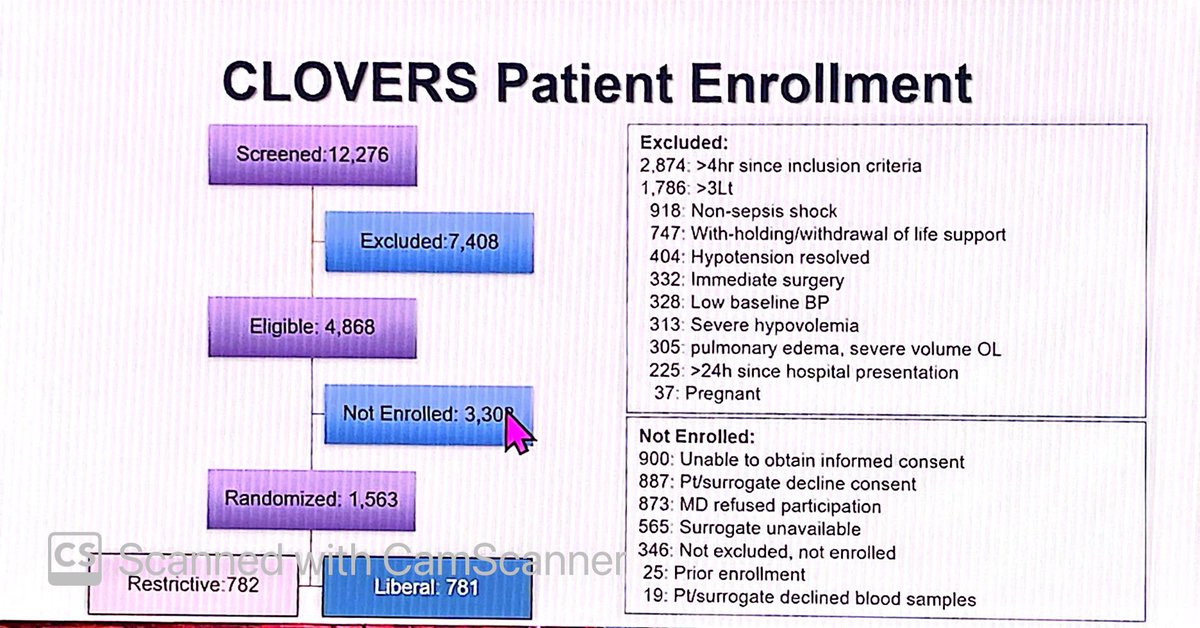
Patient characteristics #SCCM2023 

These slides show that they did indeed have a difference in therapies given. #SCCM2023 





My next #SCCM2023 tweetucation session is “Late-Breaking Studies That Will Change Your Practice”!
First we have Dr. Ivor Douglas (@com543) with “Restrictive vs Liberal Fluid Management for Sepsis-Induced Hypotension”! #SCCM2023 

So what is the optimal fluid resuscitation strategy in shock? #SCCM2023 

Jan Claassen on coma (#SCCM2023)
Above true coma there is
Vegetative: no evidence of awareness of self/environment although may open eyes (distinct from coma)
Minimally conscious state: reproducible but inconsistent awareness
Can have a higher level of MCS + command following
Above true coma there is
Vegetative: no evidence of awareness of self/environment although may open eyes (distinct from coma)
Minimally conscious state: reproducible but inconsistent awareness
Can have a higher level of MCS + command following
Locked in syndrome: paralysis of limbs and lower cranial nerves, usually still has vertical eye movements (ask them to move their eyes up and down) and eyelid opening.
Unclear when prognostic scores predict recovery, as most allowed withdrawal of care in the studies, creating self-fulfilling prophecies.
Estimated that 64% of cardiac arrests with withdrawal of care could have have subsequent functional recovery.
Estimated that 64% of cardiac arrests with withdrawal of care could have have subsequent functional recovery.
Next up for tweetucation at #SCCM2023 is “The Intersection of Climate Change and Critical Care” with Dr. Srinivas Murthy (@srinmurthy99) and Dr. Gloria Rodriquez-Vega!
We will talk about whether our ICUs are ready and what they can do to help. #SCCM2023 

Case presentation - this is a code red for humanity! #SCCM2023 


My next session for tweetucation is something I’m VERY passionate about!: “Moral Injury: Don’t Just Stand There, Do Something”! #SCCM2023
First up is “Recognizing the Signs, Symptoms, and Impacts of Moral Injury” with Kimberly Ichrist (@IchristKimberly)! #SCCM2023 

The concept of moral injury is from military literature and is “a wound from doing something that violated one’s own ethics, beliefs, or attachments.” #SCCM2023