Discover and read the best of Twitter Threads about #neuroinflammation
Most recents (16)
B12 is an important water-soluble organic compound that plays a critical role in the health of our brains. It is involved in DNA synthesis, methylation, and cellular metabolism, which means it is necessary for the proper functioning of our cells. (1/21)
B12 deficiency is a major concern, as it can lead to megaloblastic anemia and neurological problems. But did you know that inadequate #B12 or subclinical deficiency is also very common? (2/21)
It's seen at all ages but definitely in elderly populations. This can be particularly worrisome for those with Alzheimer's disease (AD), as several studies have shown an association between B12 deficiency and #AD. (3/21)
Medications called selective serotonin reuptake inhibitors, or SSRIs, can affect how microglia and astrocytes produce inflammatory molecules. 🧵 (1/19)
Interleukin 8, or IL-8, is a molecule that causes inflammation in the body. It is produced by immune cells in the brain called macrophages, microglia, and astrocytes. (2/19)
IL-8 can either help or hurt the body's response to inflammation, depending on how much is present. IL-8 is complicated. It can have neuroprotective or neurotoxic roles. (3/19)
Ketogenic diets have neurotransmitter-balancing effects. Let's do a short thread on one of my fav NTs called GABA. 🧵
GABA makes you chill out. It relaxes your mind and reduces your sense of being overwhelmed. It reduces anxiety. It helps you digest your food and actually improves gut motility and, thus, gut health because it's used to keep your parasympathetic nervous system humming along.
It also helps reduce a little something called #neuroinflammation, which, if you have any kind of mood disorder, might very likely be an issue for you.
Someone DM'd me about POTS and long-Covid and asked if a ketogenic diet could help. So let's do a quick little thread. 🧵1/7
I wrote an article about how #Keto can help with neuro #Covid symptoms, but it is mostly focused on cognitive and mood symptoms, not POTS. Here it is if anyone is interested. 2/7
mentalhealthketo.com/2022/10/01/bes…
mentalhealthketo.com/2022/10/01/bes…
That said, the mechanisms can be similar. For example, #neuroinflammation (which keto is great for) impairs the function of the #Vagus nerve, which is implicated in POTS symptoms. 3/7
Stabilization of #mastcells inhibits bacteria induced #neuroinflammation #MCAS pubmed.ncbi.nlm.nih.gov/31130850/
1/2 Microglia are the immune system of the brain. Researchers set out to discover if injecting the outer membrane of bacteria called LPS into mice triggered mast cells to activate microglia, contributing to neuroinflammation.
2/2 The determined bacterial LPS caused #mastcellactivation and cognitive impairment. The researchers also found the use of #cromolyn effectively stabilized mast cells and neuroinflammation and memory dysfunction.
A few years ago i used to do my own #research, did proteomic analysis of mouse brain, was searching for molecules which are important for neuroplasticity and published those data. 👇🏻 but today … 🧵
1/7
pubmed.ncbi.nlm.nih.gov/27062398/
1/7
pubmed.ncbi.nlm.nih.gov/27062398/
After two Sars-Cov-2 infections, i am a #longcovid sufferer and have to take care on my own brain because #brainfog and #Dysautonomia #pots #fatigue #PEM
2/7
2/7

As a #scientist i teached bachelor students in lectutes and in a practical way during experiments,
as a #longcovid sufferer i „teach“ other longhaulers about symptoms and off-label therapy options
3/7
as a #longcovid sufferer i „teach“ other longhaulers about symptoms and off-label therapy options
3/7
A significant number of COVID19 patients develop '#longCOVID', a condition defined by long-lasting debilitating, often neurological, symptoms. The pathophysiology of long COVID is unknown. 1/
Here comes a new Preprint that presents in-vivo evidence of widespread #neuroinflammation in long COVID, using a quantitative assessment, [18F]DPA-714 PET, in two long COVID patients. 2/
Excited to share our new paper out at @NatImmunol today! We discovered the limiting factor for #brain #Tregs is #IL2, and developed a new #genetherapy to treat #traumaticbraininjury and other #neuroinflammatory pathologies. 1/12
nature.com/articles/s4159…
nature.com/articles/s4159…
The work started more than 10 years ago, after my brother Russell died following a #traumaticbraininjury. The more I read into it, the more treatable #neuroinflammation seems. Obviously there is a #brain delivery problem, but stopping #inflammation is basic #immunology! 2/12 

We had a great post-doc, @EmanuelaPasciu1, drive a project showing #Tcells in mouse and human brain, with key functions. Among these T cells were a small population of anti-inflammatory #Tregs, again in mouse and human. 3/12
cell.com/cell/fulltext/…
cell.com/cell/fulltext/…
Was hat der #Darm eigentlich mit dem #Gehirn zu tun?
Neben der Verdauung und dem großen Anteil am #Immunsystem besitzt der Darm – nach unserem 🧠 – das größte #Nervensystem
Es besitzt ca. 100 Millionen Nervenzellen & ist über die #DarmHirnAchse eng mit dem ZNS verbunden.
🧵
Neben der Verdauung und dem großen Anteil am #Immunsystem besitzt der Darm – nach unserem 🧠 – das größte #Nervensystem
Es besitzt ca. 100 Millionen Nervenzellen & ist über die #DarmHirnAchse eng mit dem ZNS verbunden.
🧵

2. „Der Darm ist, neben der Haut, unser größtes Organ. Allein die Fläche des Dünndarms entspricht einem 1-Zi-Apartment (30-40 m2)“
Stoffe* aus dem Darm wirken sich potentiell auch auf das 🧠 aus.
#Neuroinflammation
* Entzündungsmediatoren, Toxine, mikrobielle Faktoren
Stoffe* aus dem Darm wirken sich potentiell auch auf das 🧠 aus.
#Neuroinflammation
* Entzündungsmediatoren, Toxine, mikrobielle Faktoren

Die #Mastzelle
➡️ Von der Medizin völlig unterschätzt und kaum beachtet.
Dabei kämpft sie direkt an der Front, in der allerersten Reihe und mit unzähligen Waffen.
🤜🏻🦠
Sie ist eine #Immunheldin - bei #MCAS leider etwas außer Rand & Band.
🧵
➡️ Von der Medizin völlig unterschätzt und kaum beachtet.
Dabei kämpft sie direkt an der Front, in der allerersten Reihe und mit unzähligen Waffen.
🤜🏻🦠
Sie ist eine #Immunheldin - bei #MCAS leider etwas außer Rand & Band.
🧵
Das entspricht (ungefähr) dem med. Standardwissen über sie:
„Eine Mastzelle ist eine zu den Leukozyten gehörende Blutzelle. Sie reift aus hämatopoetischen Stammzellen im Knochenmark heran… Sie wird IgE-vermittelt aktiviert (Allergien)…“
flexikon-mobile.doccheck.com/de/Mastzelle
„Eine Mastzelle ist eine zu den Leukozyten gehörende Blutzelle. Sie reift aus hämatopoetischen Stammzellen im Knochenmark heran… Sie wird IgE-vermittelt aktiviert (Allergien)…“
flexikon-mobile.doccheck.com/de/Mastzelle
Das ist, was sie eigentlich kann und macht. Denn getriggert wird sie längst nicht nur durch #IgE und sie sezerniert weit mehr als nur #Histamin.
Quelle: ruhtenberg.info/mcas/
Quelle: ruhtenberg.info/mcas/

This is the most straightforward explanation for chronic symptoms in at least a subset of #LongCovid patients. Partly b/c if the #virus is still present its activity can directly contribute to other phenomena also being documented in LongCovid
2/ Persistence of #SARS-CoV-2 in tissue could lead to shedding of spike protein into blood, which can catalyze the ongoing formation of microclots and hyperactivated platelets
3/ Persistence of SARS-CoV-2 can lead to ongoing downregulation of interferon and/or T cell signaling by the virus, creating an optimal atmosphere for activation of EBV or other #pathogens normally controlled by such immunity
Dr. @eyolab is presenting now! #BIIAtTheBench
@eyolab Some cool transcriptional data from this paper today: pubmed.ncbi.nlm.nih.gov/29861285/ #BIIAtTheBench #BIIW21
@eyolab A great PI goes where the data go! Integrated #SexDifferences because a trainee brought compelling data for #P2RY12 gene! #BIIW21 #BIIAtTheBench
In a meeting I watched today, microglia priming was mentioned in #LongCovid and #ME/CFS. It’s important to clarify what “microglia priming” means. Microglial priming does not mean that after a trigger has “cleared” microglia remain perpetually activated
2/ Instead, microglia priming goes like this 👉 When microglia or other glial cells detect #infection, injury, or inflammatory mediators, they enter a state of activation in which they change morphology and release their own neuroexcitatory inflammatory mediators
3/ Then, after activating, they retain a “primed” functional state which causes an even more robust response to *subsequent* infectious/immune/#inflammatory challenges. And as cells, microglia live long lives (they are not replaced as often as many other cell types)
#BHB inhibits #inflammasome activation to attenuate #Alzheimer’s disease #pathology | Journal of #Neuroinflammation |
“Here, we find BHB levels are lower in red blood cells and brain parenchyma of AD patients when compared with non-AD controls... jneuroinflammation.biomedcentral.com/articles/10.11…
“Here, we find BHB levels are lower in red blood cells and brain parenchyma of AD patients when compared with non-AD controls... jneuroinflammation.biomedcentral.com/articles/10.11…
...Furthermore, exogenous BHB administration reduced plaque formation, microgliosis, apoptosis-associated speck-like protein containing a caspase recruitment domain (Asc) speck formation, and caspase-1 activation in the 5XFAD mouse model of AD.”
“Taken together, our findings demonstrate that BHB reduces AD pathology by inhibiting NLRP3 inflammasome activation. Additionally, our data suggest dietary or pharmacological approaches to increase BHB levels as promising therapeutic strategies”
Yet another team ties #neuroinflammation to persistent brain infection 👉 Here, RNA seq + western blot + antibody testing identified pegvirus inside the #brain cells of two patients who died from encephalitis (and not controls): folio.ca/u-of-a-scienti… 


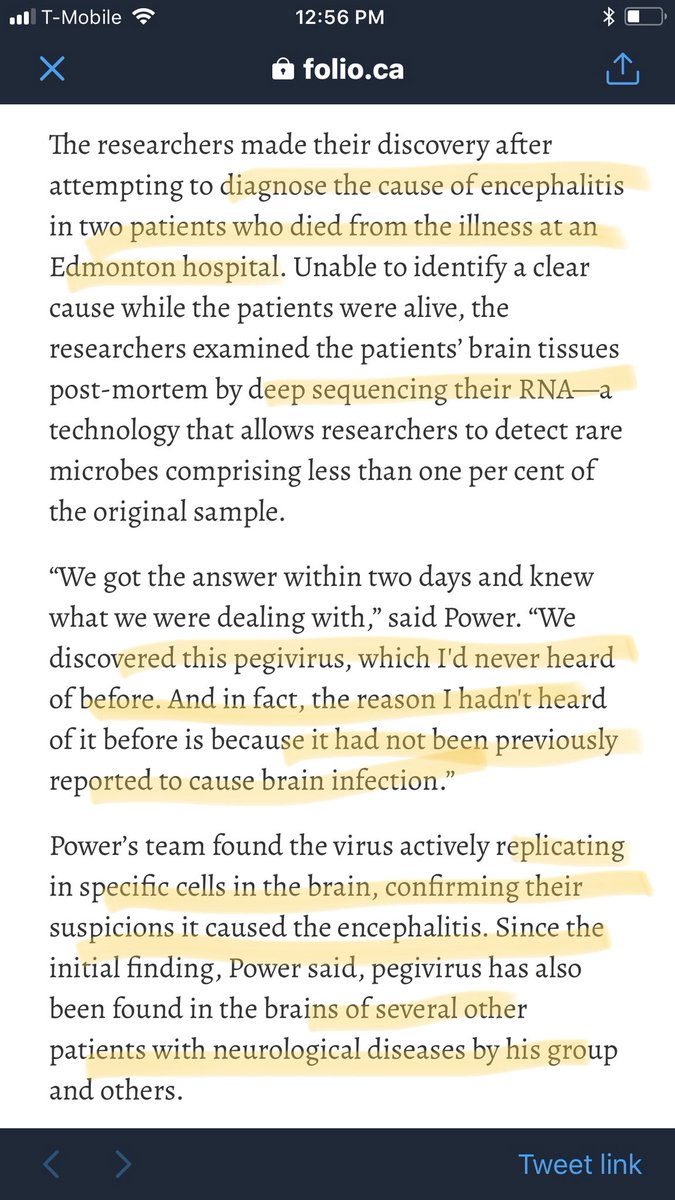
Important that pegvirus acted as an intracelluar #pathogen (viral antigens were found inside glial cells + lymphocytes + astrocytes)☝️..w/ their presence in lymphocytes suggesting the “cells might serve as a Trojan horse for #viral infection of the brain parenchymal cells.” 

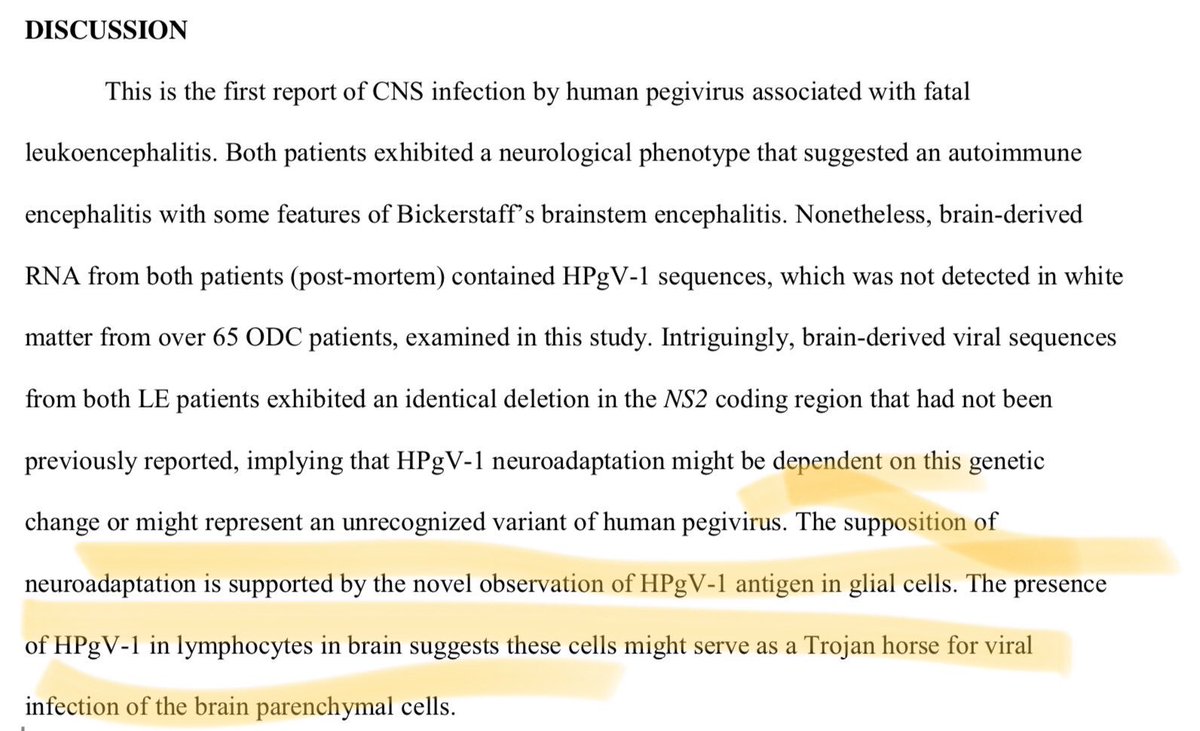

Also important is that detection of #pegvirus-antigen in the pre-transplantation bone marrow biopsy of one subject 👉 “indicated that this patient was infected at least 15 years before #neurological presentation, suggesting a period of viral latency.” 

Thread:
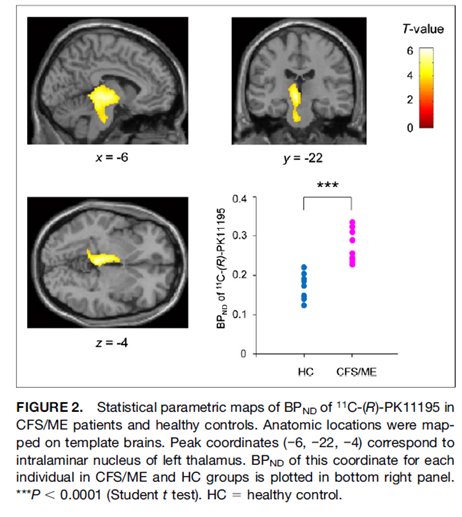
The 10 publications below provide scientific evidence that patients with #MECFS have #brain abnormalities in #neuroinflammation, #metabolism, #neurological connections and blood perfusion
#pwME suffer from #chronicillness
#pwME are #SickNotWeak
The 10 publications below provide scientific evidence that patients with #MECFS have #brain abnormalities in #neuroinflammation, #metabolism, #neurological connections and blood perfusion
#pwME suffer from #chronicillness
#pwME are #SickNotWeak
1. These studies “provide evidence of #neuroinflammation in #MECFS.. as well as evidence of the possible contribution of neuroinflammation to the pathophysiology of #MECFS”
#pwME
jnm.snmjournals.org/content/55/6/9…
#pwME
jnm.snmjournals.org/content/55/6/9…
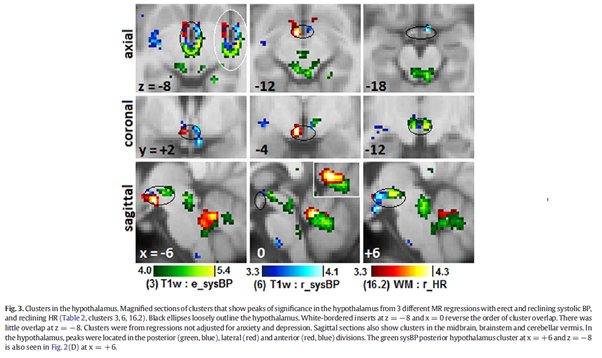
2. This Australian study found abnormalities in the #brain MRIs and peripheral Blood Pressure and Heart Rate in #MECFS patients including the Vasomotor centre, midbrain and hypothalamus
#pwME
sciencedirect.com/science/articl…
#pwME
sciencedirect.com/science/articl…